- Acne
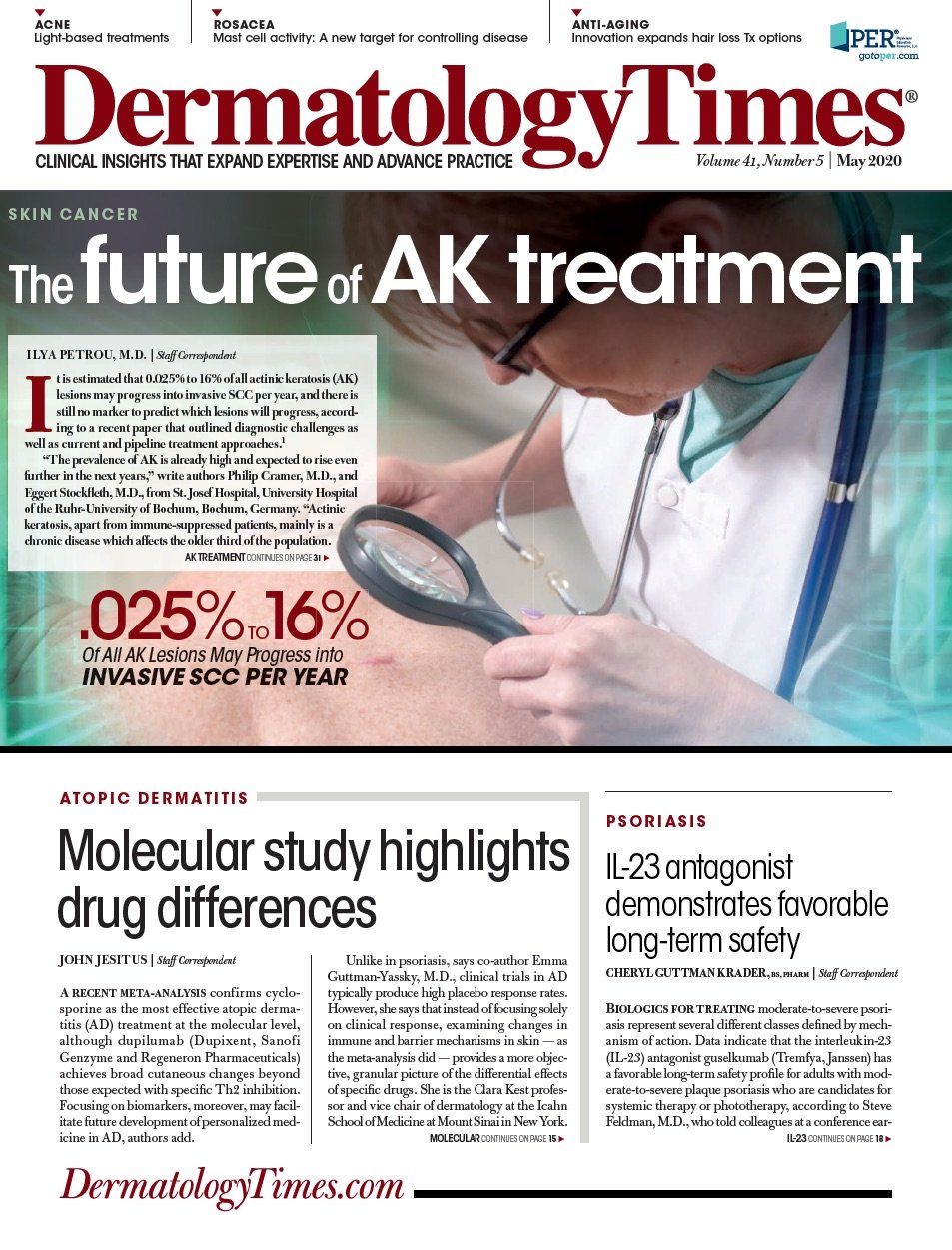
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
A new target for rosacea treatment: The mast cell
Author(s):
Recent evidence of increased mast cell activity suggests mast cell stabilization as a target for rosacea treatment.
Dr. Webster

Although it is now accepted that rosacea is a chronic inflammatory condition, the pathogenesis of this skin disease remains unclear. Complicating determination of the etiology of rosacea is the need to account for its multiple subtypes, ie., erythematotelangiectatic, papulopustular, phymatous and ocular.
RELATED: LEO Pharma’s azelaic acid foam for rosacea now available
It is likely indisputable that better understanding of rosacea etiology could offer new targets for developing better treatments, says Guy F. Webster, M.D., Ph.D., who proposes a focus on controlling mast cell activity. This concept is based on findings from several lines of research that point to a role for histamine and other chemical mediators released by mast cells.
“The clinical presentations of rosacea are diverse, but blushing resulting from an exaggerated vasodilatory response to various triggers is a shared feature among patients across the rosacea spectrum,” says Dr. Webster, Webster Dermatology, Hockessin, Del.
“If we are looking for a single way to treat rosacea, it may be time to go after the mast cell and its interactions with vascular smooth muscle and vasomotor nerves.”
The factors that can trigger a blush response in patients with rosacea include thermal change (heat) and a variety of foods. Dr. Webster cited findings reported decades ago by Jonathan Wilkin, M.D., as evidence that rosacea patients are “wired neurologically to sense temperature change and translate it into a blush.” In his research, Dr. Wilkin showed that compared with controls without rosacea, blushing in people with rosacea that occurs after drinking a warm beverage occurs with lower temperature drinks and persists for a longer duration.
Similarly, the blush reaction to various food triggers in rosacea patients is also neurologically mediated.
RELATED: Education key to optimizing care of rosacea patients
“Both heat and various dietary triggers stimulate transient receptor potential channels that are highly expressed on sensory neurons, keratinocytes and endothelial cells in the mouth and skin of rosacea patients,” Dr. Webster explains.
THE MAST CELL CONNECTION
Looking at the foods that are leading causes of the blush response for rosacea patients shows histamine content as a common thread.
Dr. Webster notes that, in a survey conducted by The National Rosacea Society, yogurt, cheese, sour cream, soy, yeast extract and chocolate were some of the most common food triggers reported by rosacea patients.
“These are all fermented foods that have a relatively elevated level of free histamine that causes a vasodilatory response,” he says.
In the body, histamine plus other mediators that cause vasodilation and an inflammatory response are released by mast cells that have been shown to be increased in numbers and activity in the facial skin of patients with rosacea. Furthermore, research by Richard Gallo, M.D., Ph.D., and colleagues at the University of California, San Diego performed in a preclinical model showed that treatment with a mast cell stabilizer effectively decreased the development of rosacea-like inflammation when the animals were challenged with cathelicidin LL-37, a known enabler of rosacea pathogenesis.