- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
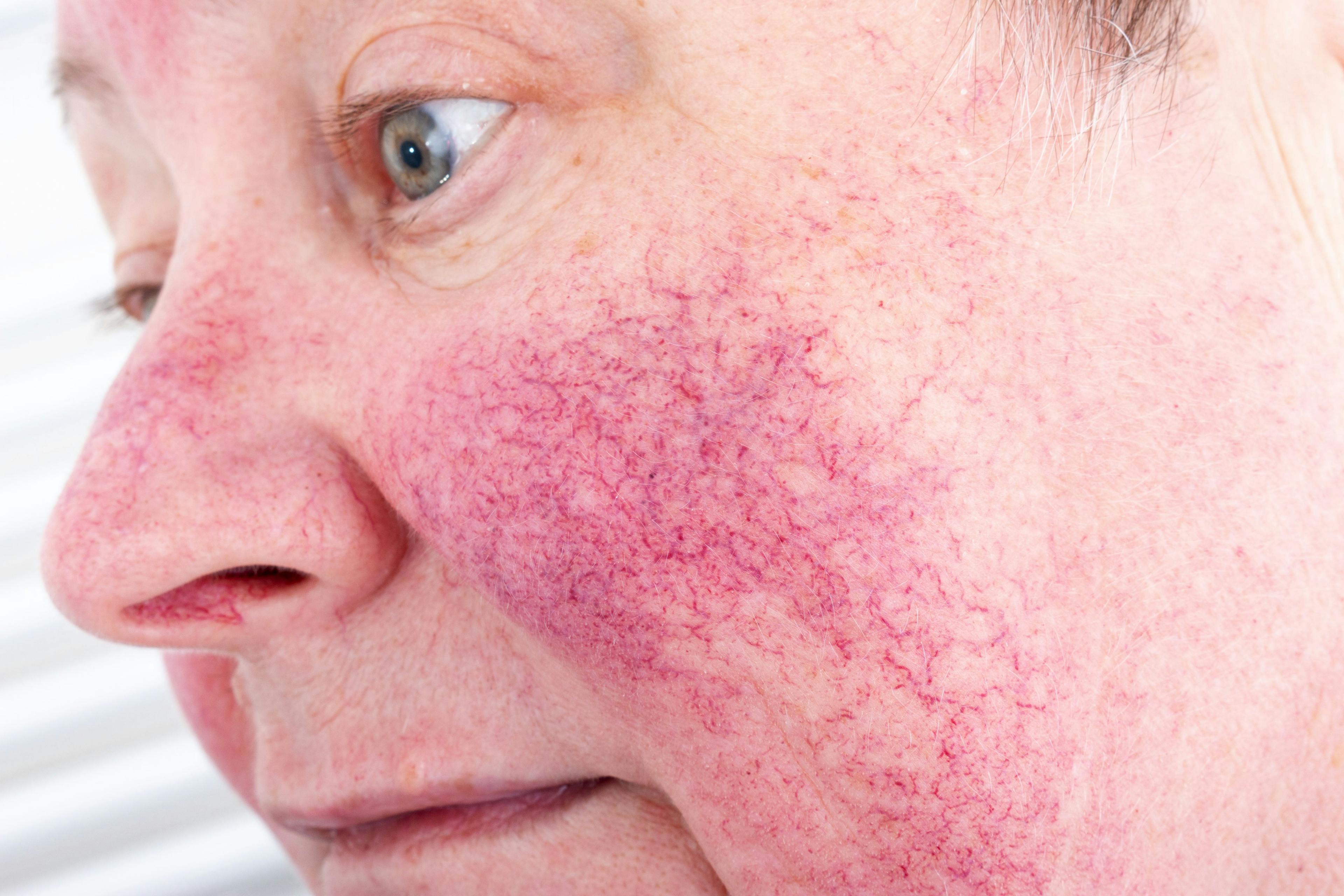
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
2021's Breakthroughs & Disappointments
Author(s):
The past year gave dermatologists ample cause for both celebration and frustration as they looked forward to new drugs, devices, and technology to optimize patient care. Here, Dermatology Times® editorial advisory board members weigh in on the good, bad, and still-TBD changes that shaped the specialty during 2021.
The Major Breakthroughs
1. FDA approval of the first topical Janus kinase (JAK) inhibitor to treat atopic dermatitis (AD). “While there were some new approvals of drugs and devices, none were really ‘breakthroughs’ with the exception of the topical JAK inhibitor ruxolitinib [Opzelura; Incyte]. This is a novel small molecule drug for a skin disease that wreaks havoc for many patients,” said Wm. Philip Werschler, MD, founding member of Spokane Dermatology Clinic and Werschler Aesthetics, both located in Spokane, Washington.
Christopher Bunick, MD, PhD, an associate professor of dermatology at Yale University School of Medicine in New Haven, Connecticut, agreed. “I think having a topical JAK inhibitor approved by the FDA, even with the class acquiring the appropriate black box warning, is a breakthrough. It signals a new era of an entire class of medications just emerging in dermatology,” he said. “This will be a hot trend line for several years, barring unforeseen adverse events [AEs].”
Patricia Farris, MD, a dermatologist at Sanova Dermatology in Metairie, Louisiana, called this topical a game changer not only for AD but also possibly for vitiligo and other conditions.
2. Advances in identifying and targeting abnormalities in cytokine pro- files that will also reduce AEs. “One of this year’s breakthroughs for psoriasis is the demonstration that [the] topical nonsteroids roflumilast [ARQ-151; Arcutis Biotherapeutics] and tapinarof (GSK2894512; Dermavant) are as effective as potent steroids without local irritation or steroid [AEs],” said Mark G. Lebwohl, MD, dean for clinical therapeutics, and chairman emeritus at the Kimberly and Eric J. Waldman Department of Dermatology, Icahn School of Medicine at Mount Sinai in New York, New York, adding that current research on targeting various pathways also could bring new options for treating alopecia areata, vitiligo, hidradenitis suppurativa, and other skin disorders.
3. New drugs that take aim at the root cause of skin disorders. FDA approval for a new nonantibiotic acne topical medication with a novel mechanism of action. “Clascoterone 1% cream [Winlevi; Sun Pharma] is a significant new agent for treating acne,” said Ranella Hirsch, MD, president of Skincare Doctors and cofounder of Atolla (now part of Function Beauty) in Boston, Massachusetts. “Its ability to reduce sebum production by targeting androgen receptors of the sebaceous glands also yields a decrease in inflammation and offers a topical antiandrogen treatment option, which previously was only achieved by medications taken orally.”
“We should see the approval of more JAK inhibitors signaling the most important advancement in anti-inflammatories since corticosteroids were invented. We are going to see the expansion of biologics into other disease indications where treatments did not previously have good therapies,” says Zoe Diana Draelos, MD, an adjunct assistant professor of dermatology at Duke University School of Medicine in Durham, North Carolina, and chief medical editor of Dermatology Times®.
4. Noninvasive solutions for aesthetic dermatology. “[Using] ultra-sound for filler complications and new techniques in filler placement appear to be revolutionary steps in improving safety,” said Mat- thew Elias, DO, FAAD, cofounder of Elias Dermatology in Fort Lauderdale, Florida, and an incoming member of the Dermatology Times® editorial advisory board.
5. Telehealth. “While I wouldn’t say telehealth is a breakthrough in itself, as it’s been used for several years, 2021 did create breakthroughs in the ways in which it is integrated into the practice. And, too, the technology to support it has come a long way over the last year,” said Amy Spizuoco, DO, a dermatologist/dermatopathologist at True Dermatology in New York, New York, and an incoming member of the Dermatology Times® editorial advisory board.
“The rise of telehealth has changed the way we can interact, engage, and follow up with patients. It allowed for a huge increase in touchless patient consultation at their time and discretion,” noted Deanne Mraz Robinson, MD, chief medical officer of Ideal Image, cofounder of Modern Dermatology PC in New York, New York, and an incoming member of the Dermatology Times® editorial advisory board.
“Telehealth did not have much impact on my procedural practice because at the end of the day, I can’t teleport a laser pulse,” Hirsch said. “But for patients, it was incredible to be able to access care, especially routine maintenance care, on a schedule that didn’t mean missing work, didn’t require a babysitter, and allowed for a much faster [visit] in most cases.”
The advent of virtual health care also sparked a breakthrough in meet- ing the demand gap for dermatologic services. “Telemedicine has become an antiquated and inappropriate term,” added Will Kirby, DO, FAOCD, chief medical officer of LaserAway in Beverly Hills, California, and an incoming member of the Dermatology Times® editorial advisory board.
“Now telehealth is more accurate. Only physicians can provide ‘medicine,’ but dermatology diagnostic and treatment care is conducted and implemented by allied health care professionals including MDs, DOs, nurse practitioners, physician assistants, and registered nurses. Telehealth helped patients—and some physicians—understand the value and contributions of all members of our health care community.”
6. New technology in training, treatment, and diagnostics. “There is so much on the horizon regarding how technology will impact dermatology, from increasing availability of less invasive technologies such as confocal in vivo laser microscopy, optical coherence tomography, and ultra-high-res US ToTo augmented reality coupled with computer vision and machine learning to provide more evidence-based guidance on prognosis and therapy, virtual reality-training, and even crowdsourcing knowledge among clinicians,” says Albert C. Yan, MD, FAAP, FAAD, chief of the section of pediatric dermatology at Children’s Hospital of Philadelphia in Pennsylvania and professor, pediatrics and dermatology, at the Perelman School of Medicine at the University of Pennsylvania.
7. COVID-19 vaccinations. “This breakthrough speaks for itself,” Elias said. Most importantly, vaccines stemmed the tide of the pandemic’s life- and health-threatening impact, he said, adding that “they allowed most dermatology practices—like other businesses—to return to some kind of normality.”
The Biggest Disappointments
1. FDA delays in approving oral JAK inhibitors for AD and, potentially, other skin disorders. “The FDA’s hold on approval of these drugs based on concerns of class-labeling [AEs] is definitely disappointing,” Werschler said.
So is the FDA decision to include topical AD treatments in the black box warning mandated for oral JAK inhibitors approved to treat conditions such as rheumatoid arthritis. “It is disappointing that the first topical JAK inhibitor carries a black box warning citing the potential risks that are usually associated with oral medications like blood clots and thrombocytopenia,” Elias said. “Patients who use topical JAK inhibitors may potentially require blood monitoring, which may limit their use among dermatologists.”
2. The FDA’s decision to decline the biologics license application of an injectable neurotoxin, daxibotulinumtoxinA (Revance Therapeutics), to treat moderate to severe glabellar lines. The FDA’s complete response letter cited factory quality control and record-keeping issues for its decision. No reference was made to deficiencies in the product.1 “Cosmetic research was dealt a serious setback with the lack of FDA approval for daxibotulinumtoxinA,” said Joel Schlessinger, MD, founder and CEO of Schlessinger MD in Omaha, Nebraska. “This may change, but it will likely send shock waves for companies that are considering toxins in the future.”
Elias added that this injectable “had the potential to revolutionize toxin treatment longevity for patients.”
3. FDA delays in device approvals. Werschler noted that stalls on Coolsculpting Elite (Allergan Aesthetics) and a new Ulthera device (Merz Aesthetics) postponed access to advances in body contouring and skin lifting, respectively.
4. Stalls in FDA action on bimekizumab (Bimzelx; UCB) and tralokinumab (Adtralza; LEO Pharma). “The former has really promising data for [positive outcomes for] skin and joints in patients with psoriasis, while the latter is a much-needed alternative for patients who do not respond to some of the current inhibitors,” Bunick said.
Lebwohl shares that disappointment. “Bimekizumab clearly works and is safe, but because of the pandemic, its approval has been delayed for more than 6 months, and we still don’t know when it will be approved,” he said. “Deucravacitinib [Bristol Myers Squibb] is highly promising and, hopefully, will get approval in 2022. But delays at the FDA are concerning.”
5. The Coronavirus Aid, Relief, and Economic Security Act’s removal of 2% hydroquinone from the marketplace. “This leaves us with no hydroquinone that is over the counter,” Schlessinger said. “More research needs to be done on marketable pigmentation agents because of this reversal. It was a terrible decision that singularly affects patients of color and should not have happened.”
6. Evolution, not revolution. “The lack of true innovation was palpable,” Mraz Robinson said. “COVID-19 slowed research and had a marked [negative] effect on product innovation because of the FDA’s past/present attention to the pandemic. And that may hamper the pipeline further.”
“From a drug and device perspective, it’s been a disappointing year,” noted Werschler.
7. Vaccine shortcomings. “The failure of the COVID-19 vaccine to provide superior immunity after 6 months is one of the biggest disappointments of the year,” Draelos said.
Reference:
1. Revance provides regulatory update on daxibotulinumtoxinA for injection for the treatment of moderate to severe glabellar (frown) lines. News release. Revance Therapeutics. October 15, 2021. Accessed November 17, 2021. https://investors.revance.com/news-releases/ news-release-details/revance-provides-regulatory-update-daxibotulinumtoxina-injection

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.