- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
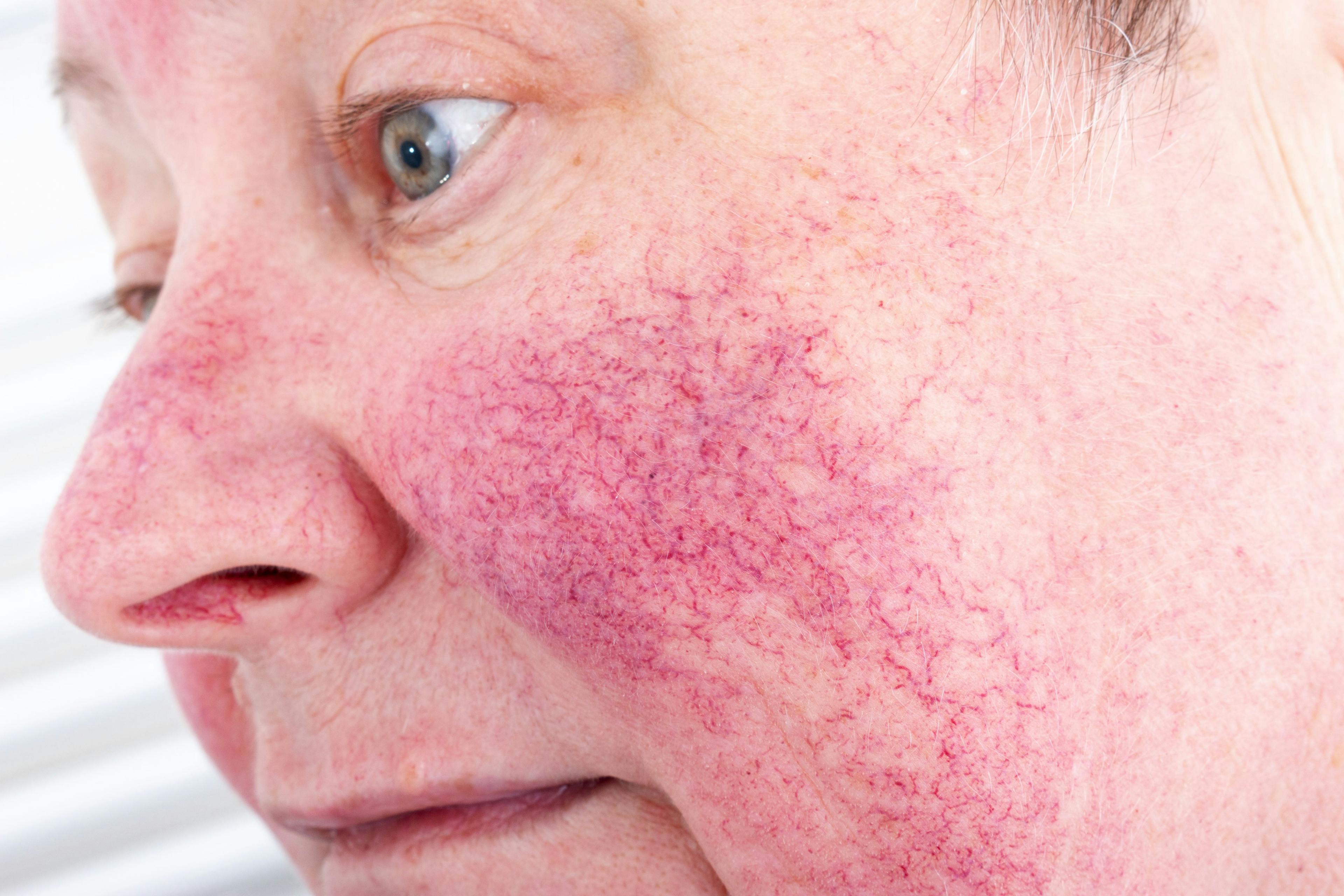
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Screening for Body Dysmorphic Disorder
Author(s):
A recent study investigates the probability of BDD in cosmetic dermatology with the help of a new screening tool.
A study published in the Journal of Cosmetic Dermatology aimed to verify the probability of body dysmorphic disorder (BDD) in cosmetic dermatology.1
BDD is defined as an obsession with a perceived defect in physical appearance that is not observable or appears slight to others. This perceived defect typically impairs a patient’s life.2
BDD is one of the most common psychiatric conditions for which aesthetic patients receive diagnoses.3 BDD involves a distorted perception of body image; consequently, aesthetic treatments and procedures can never fulfill patients’ desired but unobtainable result.
The study used a multiphasic screening protocol for BDD that was distributed to 8 medical spa clinics in the United States. The prescreening form was administered to incoming patients aged 18 to 65 years from June 1, 2019, through September 1, 2019. The patients were not made aware that they were being studied in an
attempt to avoid the low sensitivity and specificity that can occur during psychological screenings where patients are highly motivated to succeed in order to be treated.1 Medical exclusions included any procedure limitation like pregnancy or breastfeeding, allergies to the injected materials, or neuromuscular disorders. There were no exclusions based on psychological reasons.
The multiphasic portion of the study started with an informal, anonymous survey that included questions deemed useful in determining the psychological motivators for treatment. The unhealthy motivators on the checklist were: “I want to look perfect,” “I want to look 20 again,” and “I want to look perfectly symmetrical.” If any of those specific survey options were checked by patients, they were flagged and offered a secondary screening.
The second screening consisted of a modified Cosmetic Procedure Screen- ing Questionnaire (COPS). The patients were asked to describe the features they considered of most concern in order of highest priority. They were also asked 8 questions about assessing the impact of those concerns on multiple aspects of daily life.
If the results were negative for BDD, no further data were collected. If the results indicated possible BDD, the medical providers could choose to refuse treatment and the patient’s response to that denial was documented in the study notes. Any providers who opted to treat a patient with possible BDD recorded additional supplementary information, including patient outcomes, satisfaction, and emerging areas of concern.
Over the 16 weeks, 734 initial screenings were recorded. From that total, 31 patients (4.2%) continued to the COPS screening. Of the 31 patients, 9 (29%) screened positive for BDD. More than 77% (7 of 9) practitioners refused to treat after positive BDD screening.
Of the 7 patients who screened positive, 1 went on to seek a mental health specialist, 1 received a diagnosis of BDD, and underwent therapy for the condition. Another 2 patients underwent a third screening, and both were subsequently treated with positive results.
Study limitations included a small subject size, lack of patient demographics, and patient characteristics. Future studies are needed to review a larger pool of clinics for a longer period of time, increased patient population, and broadening locations criteria to a national scale. More research is also needed to verify the usefulness and validity of a multiphasic, screening protocol in aesthetic patients.
“This pilot study underscores the clinical value of a multiphasic approach to screening for BDD in an at-risk population to not only avoid unsuccessful out- comes but to adhere to the tenet of ‘do no harm,’ ” the study authors wrote.
References:
1 Fletcher L. Development of a multiphasic, cryptic screening protocol for body dysmorphic disorder in cosmetic dermatology. JCosmetDermatol. 2021;20(4):1254-1262. doi:10.1111/jocd.13885
2 Bowyer L, Krebs G, Mataix-Cols D, Veale D, Monzani B. A critical review of cosmetic treatment outcomes in body dysmorphic disorder. BodyImage. 2016;19:18. doi:10.1016/j.bodyim.2016.07.001
3 Sarwer DB, Spitzer JC. Body image dysmorphic disorder in persons who undergo aesthetic medical treatments. Aesthet Surg J. 2012;32(8):999-1009. doi:10.1177/1090820X12462715

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.