- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
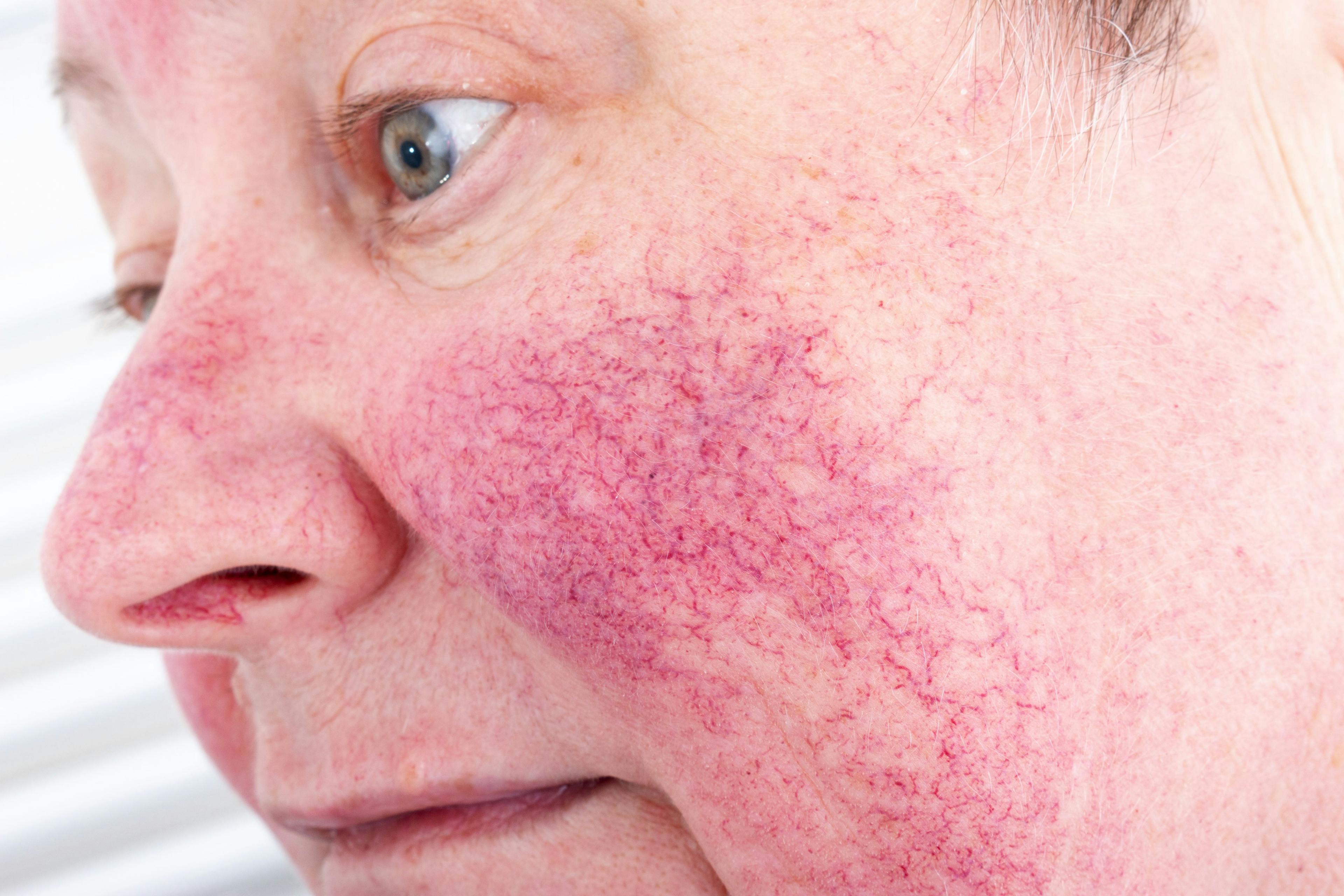
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Multimodal Plan Combats Combination Rosacea
Author(s):
Hilary Baldwin, MD, used examples of challenging cases to show how to develop successful combination regimens.
Rosacea with more than one phenotypic characteristic cannot be effectively treated with a single medication, according to Hilary Baldwin, MD, medical director of the Acne Treatment and Research Center, Brooklyn, New York, and clinical associate professor at Rutgers Robert Wood Johnson Medical Center, New Brunswick, New Jersey. During a presentation at the American Academy of Dermatology Summer Meeting, she used examples of challenging cases to show how to develop successful combination regimens.1
“When the patient has combination rosacea, you always need multiple medications or procedures,” Baldwin said. “For instance, a patient may have both background erythema and papules and pustules. Another may have some telangiectasias and some flushing, perhaps along with symptoms of stinging, burning, and itching. There is no single modality that treats all of the varied signs of rosacea. You will need at least 2 pharmacologic/procedural techniques to make that patient well.”
In the past 5 years, consensus and expert groups have advocated eradicating the subtype descriptions of rosacea. “Rather than trying to squeeze people into subtypes, we realize that most patients have a combination of signs and symptoms; a little bit of this and a little bit of that,” Baldwin said. “One of the most important reasons for doing that is that there is no single medication that makes people with a little bit of this and a little bit of that fully well.”
This new phenotypic description underscores the importance of evaluating rosacea carefully with mirror in hand, Baldwin said: “I recommend pointing out the salient features and then discussing how we can approach each aspect of the disease.”
Clinicians also should ask patients what symptom bothers them most. “Therefore, we can tailor the treatment to the patient’s specific phenotype, as well as to their needs and desires,” Baldwin said.
For primarily vascular rosacea, Baldwin uses brimonidine or oxymetazoline. In some cases, she may layer on a therapeutic modality such as laser or light-based therapy.
For papulopustular rosacea, she advised using an anti-inflammatory dose of doxycycline, topical minocycline, and/or topical ivermectin. A microencapsulated benzoyl peroxide will also soon be available, she added. For papulopustular rosacea that fails to respond to the conventional medications listed above, isotretinoin may offer an answer. “The data for isotretinoin demonstrates improvement in papules and pustules and to some extent in erythema,” Baldwin said. “Isotretinoin also has the ability to shrink phymatous tissue and prevent worsening of phymas.”
However, unlike outcomes when using isotretinoin for acne, the improvement seen in rosacea may be temporary. “Upon discontinuation of the medication, rosacea frequently returns, whereas with acne, 80% of people who use isotretinoin never see acne again,” Baldwin said. “One explanation is that isotretinoin may act as an anti-inflammatory in rosacea, so once the drug is stopped, the inflammation returns.”
Baldwin presented a case of a pregnant woman with rosacea fulminans. “Originally, the woman was misdiagnosed with acne and failed to respond to treatment,” she said. The condition progressed to involve the entire face with deep, nodules with extensive scarring but was finally treated successfully with prednisone. “In this particular case, the woman’s obstetrician was very forward-thinking and in favor of us using prednisone,” she said.
Despite the safety concerns related to prednisone, “this was one of those times when the risk-benefit ratio favored its use,” Baldwin said. “The patient’s baby was fine, although delivered 2 weeks premature. The mother was also totally healthy.”
Baldwin believes that nearly all challenging cases of rosacea can be overcome. “Sometimes you have to think outside the box, and sometimes you have to move beyond the FDA-approved therapies, including isotretinoin and prednisone,” she said. “With a combination of medications, most rosacea patients can be brought to a reasonable level of disease, if not clear.”
The treatment protocol for severe rosacea, however, may require several medications; an oral and 1 or 2 topical medications, along with a physical modality that may not be covered by insurance. “This regimen may be prohibitive in cost or beyond what the patient is willing to commit to,” Baldwin said.
Disclosures
Baldwin is an advisory board member and speaker for Galderma, Ortho Dermatologics, VYNE Therapeutics, and SUN Dermatology.
Reference
1 Baldwin H. Challenging cases in acne and rosacea. Presented at: American Academy of Dermatologists 2021 Summer Meet- ing; August 5-8, 2021; Tampa, FL.

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.