- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Ethnicity and Atopic Dermatitis: Differences, Similarities, and Gaps in Knowledge
Author(s):
There are several fine nuances and differences in the presentation of atopic dermatitis in patients with skin of color that differ from the presentation seen in patients with lighter skin types. As such, clinicians should be aware of these differences to improve the treatment and management of AD in patients with skin of color.
Although the cutaneous manifestations of atopic dermatitis (AD) may be easy to diagnose in patients with lighter Fitzpatrick skin types, the untrained eye may not be so quick to recognize this common condition in patients with skin of color (SOC). Clinicians need to closely review the key differences and subtle signs in presentation to accurately diagnose, treat, and appropriately manage AD in patients with SOC, said Ama Alexis, MD, a specialist in adult and pediatric allergy, asthma, and immunology at NYU Langone Health in New York, New York.
In her presentation at the American College of Allergy, Asthma & Immunology annual meeting in New Orleans, Louisiana, Alexis detailed how to assess AD in SOC.1
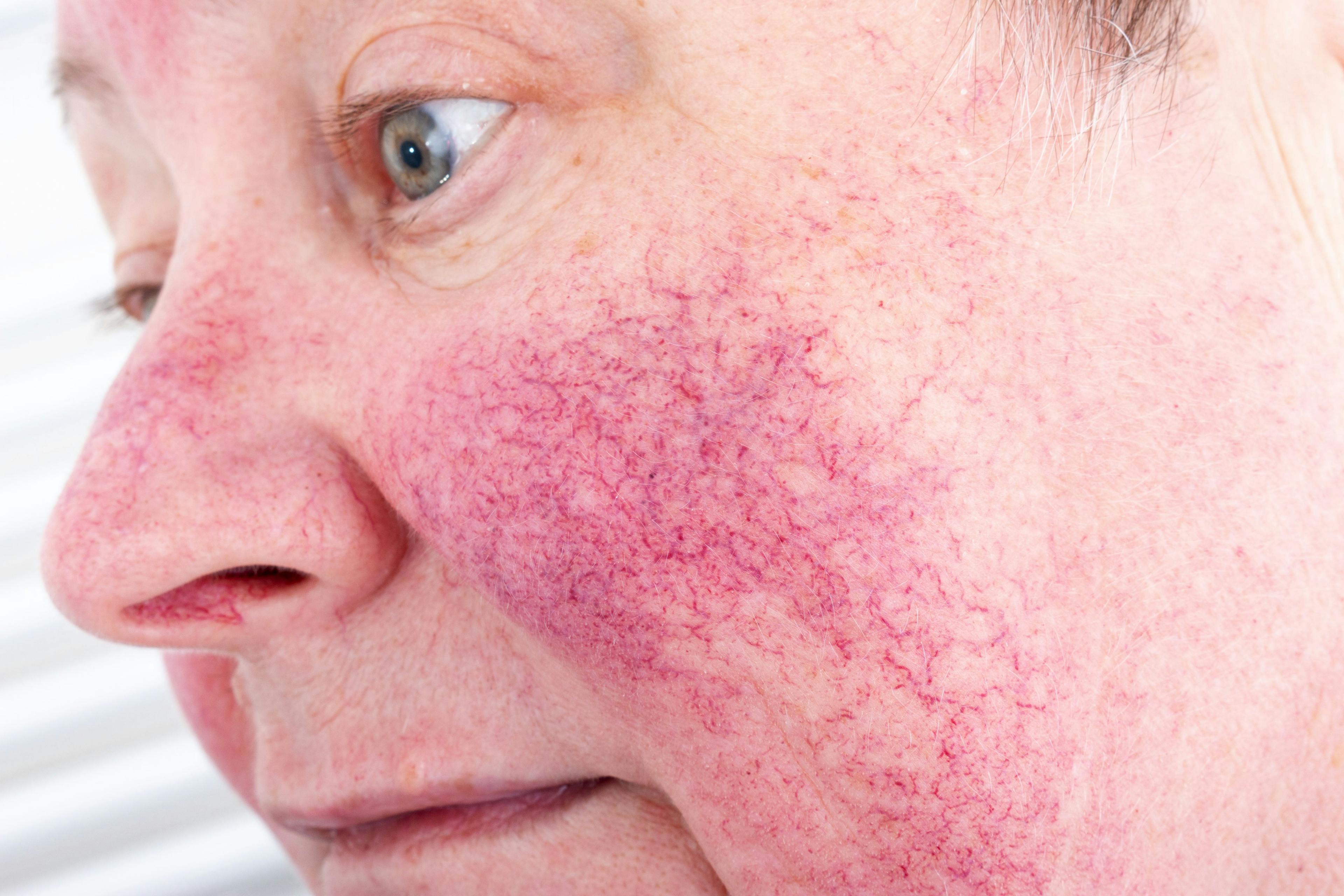
AD may present with pruritus as the hallmark symptom among all Fitzpatrick skin types, but the appearance of skin lesions can vary greatly among the phototypes. Whereas AD classically presents with erythematous patches and plaques affecting flexor surfaces in lighter skin, darker skin often presents with papules, lichenification, and pigmentary changes with more frequent extensor surface involvement.
Ama Alexis, MD, Adult and Pediatric Allergy, Asthma & Immunology, NYU Langone Health, New York, New York.

“There are a few nuances that can make it more challenging to diagnose AD in patients with [SOC] because of the altered appearance of erythema. In patients with [SOC], we do not often see bright red erythema in AD but instead shades of violet, grey or brown, and this can sometimes make it more challenging to appreciate the severity of the disease state,” said Ama Alexis, MD, who is also a clinical assistant professor in the Department of Pediatrics at NYU Grossman School of Medicine.
Other morphologic nuances in the presentation of AD in patients with SOC include perifollicular accentuation, scattered distinct papules, and differences in the distribution of skin lesions. According to Alexis, clinicians must know how to recognize and appropriately diagnose the atypical presentations of AD and then accurately evaluate its severity.
Contact dermatitis is also common in patients with SOC. Alexis said that the altered presentation and appearance of the erythema can make it difficult to read the results of patch testing accurately. Being aware of these subtleties can help improve the treatment and management outcomes in patients with darker skin types.
Despite the numerous safe and effective therapies available, patients with SOC are less likely to receive mainstream treatments such as dupilumab (Dupixent; Sanofi and Regeneron) and calcineurin inhibitors—interestingly, with the exception of hydrocortisone—than patients who have lighter Fitzpatrick skin types, showed the results of a recent review of therapies given to patients with AD.2 According to Alexis, clinicians must keep in mind that, beyond hydrocortisone, several effective and safe therapeutic options can be used for patients with SOC.
“On the one hand, we know that the prevalence and the severity of AD in patients with skin of color is higher, and on the other hand, there are disparities in the treatment, as hydrocortisone is still the most prescribed therapy, as recently published in the study by Bell et al,” Alexis said. “I believe that this is an area where we can surely improve the therapy and management of AD in our patients with skin of color.”
Despite recent progress, Alexis said, the literature lacks good clinical images for physicians who want visual examples of the differences in presentation across all skin types. “Fortunately, the gap in knowledge is closing, and there is more awareness of late,” Alexis said. “However, much still needs to be done to better serve this patient population. Just recently, the American College of Allergy, Asthma & Immunology published a [post] on their website addressing eczema in [SOC]. I believe the tide is slowly turning in terms of an increased awareness among clinicians of these disparities and the need for improved care of AD patients with [SOC].”
Clinicians should have a detailed and informative conversation with their patients who have AD, said Alexis, who explained the higher prevalence and severity of AD in patients with SOC as well as atypical presentations and areas of distribution. The discussion should aim to help each patient better understand their condition and engage them in developing a treatment regimen.
“I believe it is paramount that we educate and close that knowledge gap regarding what is, at times, different presentation of erythematous diseases such as AD in patients with [SOC],” Alexis said. “This will surely lead to improved treatment and management of this population.”
Disclosure:
Alexis reported no relevant financial disclosures.
References:
1. Ethnicity and atopic dermatitis: differences, similarities, and gaps in knowledge. Presented at: ACAAI 2021 Annual Scientific Meeting; November 4-8, 2021; in New Orleans, LA, and virtual.
2. Bell MA, Whang KA, Thomas J, Aguh C, Kwatra SG. Racial and ethnic disparities in access to emerging and frontline therapies in common dermatological conditions: a cross-sectional study. J Natl Med Assoc. 2020 Dec;112(6):650-653. doi: 10.1016/j.jnma.2020.06.009. Epub 2020 Jul 5

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.