- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Advances in Rosacea Therapy
Author(s):
April is National Rosacea Month. Recent data has indicated a correlation between rosacea and certain cardiovascular, neurologic, endocrine, and gastrointestinal disorders. Steve Daveluy, MD, FAAD shares insight on that, plus several new and exciting therapies available.
With all the recent advances in therapy for the chronic inflammatory and relapsing central facial dermatosis known as rosacea, the condition can nevertheless be very challenging to treat. Interestingly, many of the newer treatment approaches currently used in rosacea involve fine-tuning and tweaking the older medications that have already proven their therapeutic efficacy for the disease.
The precise etiology of rosacea remains unclear, with neurovascular dysregulation, activation of the immune system, and infestation with Demodex mites being among the suggested pathophysiologic mechanisms.
Subtype Presentation
According to the clinical subtype and areas involved, rosacea is typically characterized by recurrent episodes of flushing (acute or subacute intermittent vasodilation) or transient erythema, persistent erythema, phymatous changes, papules, pustules, telangiectasias, as well as local edema and pain, burning, and ocular symptoms. Approximately 50% to 75% of patients with rosacea will have ocular involvement, presenting with symptoms including dryness, redness, tearing, a tingling/burning sensation, a foreign body sensation, light sensitivity, and blurred vision.1
As the disease is very visible, it can often cause a significant psychosocial impact in patients, leading to negative consequences in quality of life such as anxiety, depression, low self-esteem, and a depreciation of general well-being, underscoring the need for more improved treatment modalities that can better control the clinical symptoms and flares of the disease as they arise.
Mainstay Medications
Whether addressing erythematotelangiectatic rosacea, papulopustular rosacea, phymatous rosacea, or ocular rosacea, clinicians now have access to a trove of therapeutic modalities and treatment approaches that can effectively address the symptoms of each subtype. To address the different clinical symptoms sometimes manifested by the disease, clinicians must often implement a combination of these therapies.
“Although we now have an increasing number of therapeutic tools and treatment modalities for the disease in our armamentarium, what’s interesting is that some of the newest therapies we have for rosacea are actually the older drugs we’ve used for the disease, with tweaks in the way these drugs are delivered to the skin,” said Steven Daveluy, MD, associate professor and program director of Wayne State University Department of Dermatology, president ofthe Wayne State University School of Medicine Alumni Board of Governors, president of Michigan Dermatological Society, and past president of the Wayne County Medical Society of Southeast Michigan in Dearborn.
The mainstay of rosacea treatment has classically been topical medications such as metronidazole 0.75% and 1% gel; azelaic acid 15% gelor 20% cream; sulfacetamide 10% and sulfur 5% lotion; tretinoin 0.25% to 1% cream; oral antibiotics from the tetracycline family; as well as the oral retinoids used alone or in combination with other treatment modalities. In addition to these approaches, other therapeutic modalities that have been effectively employed in rosacea include laser and light modalities, such as intense pulsed light (IPL) and pulsed dye laser (PDL). However, some of the exciting novel treatment approaches that have recently demonstrated significant therapeutic value include topical benzoyl peroxide (BPO), brimonidine tartrate 0.33% gel, oxymetazoline hydrochloride 1% cream, ivermectin 1% cream, tacrolimus and pimecrolimus, botulinum toxin injections, as well as submicrobiallow-dose modified release tetracyclines (ie, 40 mg doxycycline or 40 mg minocycline).
“Depending on the severity of symptoms, I will sometimes opt for the submicrobiallow-dose tetracyclines, because we know rosacea is not a bacterial issue but an inflammatory one. Therefore, it is the anti-inflammatory effect we want so we can lower the [adverse]effects of the oral antibiotic, particularly in patients who may require long-term therapy,” Daveluy said.
Newer treatments for rosacea such as topical microencapsulated BPO (Epsolay 5% cream; Sol-Gel Technologies, Ltd/Galderma), combination microencapsulated BPO 3% and microencapsulated tretinoin 0.1% (Twyneo; Sol-Gel Technologies, Ltd), and the still off-label use of the topical retinoid trifarotene 0.005% cream (Aklief; Galderma) are a very welcomed addition to the dermatologic armamentarium for patients with rosacea. Traditionally, these agents were too irritating for the typically sensitive rosacea skin, and any kind of irritation could quickly trigger a flare of symptoms, Daveluy explained. The newer fine-tuned formulations of these agents using microencapsulation technology, or nanoparticles, allow for a slow release of the drug, largely circumventing any irritation of the skin while maintaining their therapeutic effects.
“Although the [mechanism of action] of these agents should be useful for rosacea, we could never really use them very effectively or efficiently due to the irritation they so often caused. Instead of applying these topicals with a high concentration of the drug, quickly getting in the targeted skin and causing irritation—which can often lead to cessation of treatment—it is this slower and controlled release of the product that can help avoid that irritation and allow the drug to be applied regularly, with excellent clinical outcomes,” Daveluy said.
The Skin Microbiome
Similar to Demodex folliculitis, an infestation of the Demodex mite has been implicated as a possible cause of rosacea, and topical ivermectin has proven to be useful in quelling symptoms, according to Daveluy. Here, however, the question of pathogenesis remains as to whether the Demodex mite triggers rosacea or the presence of rosacea increases the Demodex mite population, leading to rosacea symptoms.
“In some cases, I may prescribe a short course of oral ivermectin, then follow-up with topical permethrin 5% cream once or twice a week. This treatment regimen has also shown to work very well in rosacea. Although permethrin is used off-label here, fortunately, it usually gets covered by insurances without much issue,” Daveluy said.
For the traditional papulopustular rosacea subtype, Daveluy will often use topical metronidazole, azelaic acid, and the oral tetracyclines. For the erythematotelangiectatic subtype, the alphaagonists including brimonidine and oxymetazoline, as well as diverse laser modalities, have shown to be very effective in addressing the persistent erythema and flushing components of the disease. If patients present with multiple subtypes, combination therapy is often required to address the different clinical aspects of rosacea.
Best Practices
“Some patients will successfully clear their rosacea symptoms with topical brimonidine or oxymetazoline, [but] they may still not be happy with clinical outcomes because their background rosacea-associated telangiectasias may be unmasked, which will then require other treatments, such as PDL therapy. As such, combination therapy is very often the order of the day in patients who present with multiple symptoms of rosacea,” Daveluy said.
When addressing the telangiectatic aspect of rosacea, IPL can be effective,but lasers are very often the treatment of choice. Instead of IPL therapy, Daveluy will often opt for PDL 585 to 595 nm or neodymium-doped yttrium aluminum garent treatment in his patients with rosacea, as the laser device is more effective at targeting hemoglobin, the specific targeted chromophore. “I prefer using the PDL. Once you get comfortable with the device, you can tweak it with different settings and use different tips to better target the telangiectasias and the background erythema with really good results,” Daveluy said.
In addition, PDL therapy is a relatively inexpensive treatment (approximately $150 to $200 per session), Daveluy added, and patients will usually only require a single treatment to clear their telangiectasias. However, patients may return for a repeat treatment over the years, if needed, as their redness may return. It is very important to inform patients of the fairly low cost of PDL therapy, as well as the 1-off PDL treatment to clear their erythema, as many patients are under the impression that laser therapy can be very expensive and out of their financial reach, Davelut explained.
Patients with rosacea should always be appropriately screened for ocular symptoms, as it is not uncommon that they are acutely aware of their rosacea-associated eye symptoms. Patients with ocular rosacea symptoms can be given cyclosporine 0.05% eye drops once every 12 hours, fusidic acid gel or metronidazole 0.75% gel applied 1 to 2 times daily on the eyelids, and in more severe cases, a low-dose oral tetracycline regimen may be required, according to Daveluy.
“A multidisciplinary approach is not always needed, [but] it depends on the severity of symptoms. Often, patients do not complain about eye symptoms, but when you ask them, they might tell you there is some dryness or irritation in their eyes. In more severe cases where they may develop styes, I will refer them to an ophthalmologist for further evaluation and treatment,” Daveluy said.
Patient’s Role in Management
One of the most important proactive steps that patients can take to keep their rosacea in check and help avoid symptoms and flares is to identify and avoid the triggering factors of the disease, which include ultraviolet light, certain spices, weather changes, and alcoholic beverages. In addition, patients should practice daily gentle skin care, including the use of pH-balanced skin cleansers (nonsoap cleaners), broad-spectrum sunscreen with SPF 30 or higher, and regularly apply skin moisturizers.2
Thephymatous component of rosacea is most commonly seen in men and can be challenging to treat.3 Therapy with oral and/or topical medication earlyon can be useful in slowing down or stopping the phymatous changes, which are most typically seen on the nose. Noticing the subtle phymatous changes on the nose earlyon allows clinicians to address them with medications like tretinoin before it progresses to the next stage of overt rhinophyma, where laser therapy including carbon dioxide and erbium laser platforms have now become the treatment of choice.4
“Electrocautery dermabrasion has taken the backseat with the advent of the [carbon dioxide] and erbium laser technologies. These laser treatments are very rewarding because it is so tough for the patients to psychologically deal with this aspect of rosacea, and there is a quick payback with laser therapy,” Daveluy said.
In terms of prevention and avoiding triggers, there is a postulated theory that treating the telangiectatic blood vessels in rosacea can help reduce inflammation, according to Daveluy. Therefore, if patients undergo laser therapy early on in their treatment course, it might also help keep the papulopustular subtype of rosacea at bay.
The treatment and management of rosacea typically involves a multifaceted approach, but patient education in rosacea remains crucial. In addition to patients seeking out helpful information from dedicated sites such as the National Rosacea Society, it is also the responsibility of physicians to appropriately educate their patients on all aspects of rosacea, including patient expectations from therapy, particularly when it comes to the triggers of the disease.
Comorbidities
Recent studies have indicated a possible correlation of rosacea with neurologic, cardiovascular, endocrine, and gastrointestinal comorbidities.5,6 Particularly true for the erythematotelangiectatic subtype with flushing, patients with rosacea have been associated with an increased risk for clotting events such as stroke. As such, Daveluy said it is important to appropriately inform patients with rosacea about this possibility—without scaring them.
“Although it is not a very big risk, patients [must] be informed that rosacea does come with an increased risk of cardiovascular disease and stroke, so you want to be sure to…cover your bases to optimally care for your patients. At this point, it is also a good idea to be sure they have a primary care physician [who] is looking after them, as well. This will help them mitigate their risk and keep their cholesterol and blood pressure in check—very similar to our [patients with] psoriasis,” Daveluy said.
Disclosures: None relevant
PATIENCE IS KEY
Zoe Diana Draelos, MD, and editor in chief of Dermatology Times® offered her pearls on the treatment management of the various subtypes of rosacea. She noted that patient adherence is crucial to treatment to the point of control, which has prompted the National Rosacea Society’s 2023 Theme “Give New Treatments Time to Work.”
“It's important to recognize that rosacea is a chronic disease. And because it's a chronic disease, it requires continued treatment. One of the goals of treatment is to prevent rosacea from worsening from going from the erythematous stage to the inflammatory, papulopustular stage and avoiding the rhinophyma stage. So, adherence is really important because it's different than treating an acute infection.”
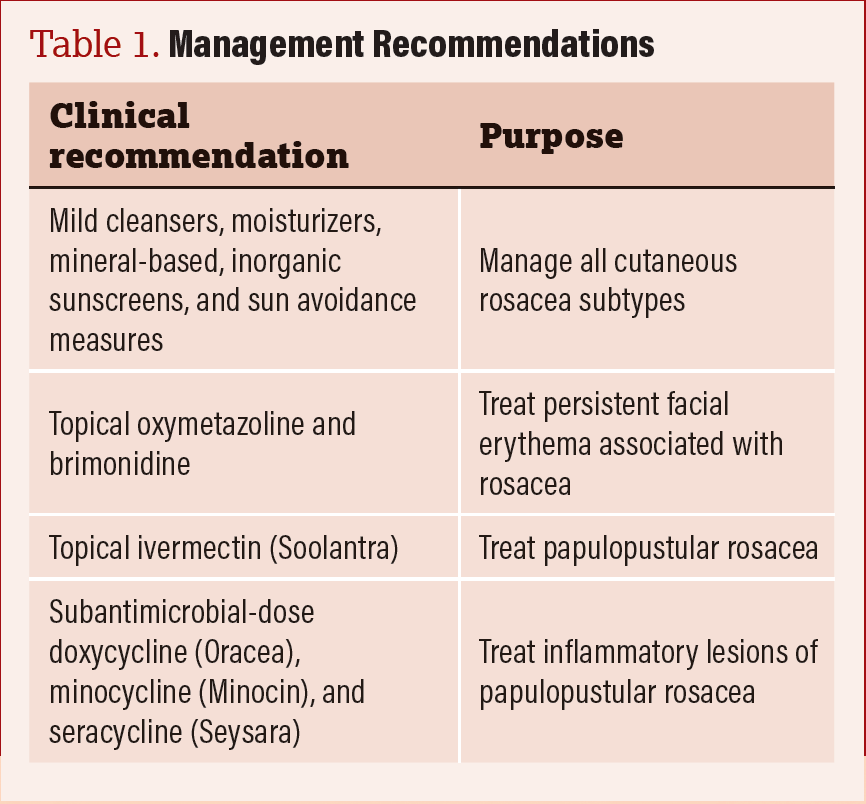
Draelos said successful treatment is pharmaceutical and cosmetic skincare products combined together to yield a much better outcome for the patient (Table 1).
Table 1. Zoe Draelos shares rosacea management recommendations.
Table 1
References
- Mehdi F, Daveluy S. Rosacea. StatPearls Publishing LLC; 2022.
- HOW TO PREVENT ROSACEA FLARE-UPS . American Academy of Dermatology Associatin. https://www.aad.org/public/diseases/rosacea/triggers/prevent. Accessed March 20, 2023.
- Rivero AL, Whitfeld M. An update on the treatment of rosacea. Aust Prescr. 2018 Feb;41(1):20-24. doi: 10.18773/austprescr.2018.004. Epub 2018 Feb 1. PMID: 29507456; PMCID: PMC5828925.
- Farshchian M, Daveluy S. Rosacea. [Updated 2022 Sep 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557574/
- Holmes AD, Spoendlin J, Chien AL, Baldwin H, Chang ALS. Evidence-based update on rosacea comorbidities and their common physiologic pathways. J Am Acad Dermatol. 2018;78(1):156-166. doi:10.1016/j.jaad.2017.07.055
- Haber R, El Gemayel M. Comorbidities in rosacea: a systematic review and update. J Am Acad Dermatol. 2018;78(4):786-792.e8.doi:10.1016/j.jaad.2017.09.016

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.