- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Merkel Cell Polyomavirus and Associated Merkel Cell Carcinoma
Author(s):
Merkel cell carcinoma is a rare but highly aggressive type of nonmelanoma skin cancer and Merkel cell polyomavirus is thought to play a major role in its etiology.
Merkel cell carcinoma (MCC) is a rare but aggressive neuroendocrine tumor of the skin carrying a high risk of recurrence and metastasis. This rare nonmelanoma skin cancer has notoriously been challenging to treat, with truly effective therapies few and far between. Continued research however has resulted in a better understanding of its pathogenesis and oncogenic mechanisms and has led to novel treatments including immune-based therapies. A recent study1 reviewed the current knowledge of MCC and the progress made in elucidating both the natural host of Merkel cell polyomavirus (MCPyV) infection and the cell of origin for MCC, as well as insights into potential targeted therapies for the disease.
Most frequently seen on the head and neck region of elderly, white males, the major risk factors for MCC include excessive ultraviolet (UV) exposure, advancing age, and immunosuppression. Nearly all healthy adults asymptomatically shed MCPyV from their skin however in the elderly and immunosuppressed population, the infection can lead to the development of the deadly tumor.
Presenting non-specifically as rapidly growing, red to violaceous nodules on sun-exposed areas, the definitive diagnosis of MCC can be made through a skin biopsy and immunohistochemical staining for markers such as cytokeratin-20 (CK-20). Differential diagnoses for MCC include basal cell carcinoma (BCC), melanoma, squamous cell carcinoma (SCC), dermatofibroma, keratoacanthoma, and cutaneous manifestations of metastatic carcinomas.
Merkel cell polyomavirus is an unenveloped double-stranded DNA virus of the family of polyomaviruses. The virus has been strongly linked to the development of MCC, with approximately 80% of cases caused by MCPyV infection and 20% from UV radiation exposure.
“Merkel cell carcinoma was initially believed to originate from Merkel cells, a rare population of mechanoreceptor cells within the epidermis. After the discovery of MCPyV in 2008, the evidence quickly arose that MCPyV establishes asymptomatic and persistent infection in a large proportion of the human population, with initial exposure often occurring during early childhood and a seroprevalence that increases among older age groups,” wrote Jianxin You, PhD, associate professor of microbiology, department of microbiology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, and co-author of the study.
Candidates for the MCC cell origin include Merkel cell precursors, epithelial stem cells, dermal mesenchymal cells, human dermal fibroblasts, and pro-B or per-B cells. According to the authors, study observations suggest that MCPyV that have replicated in the dermal cells surrounding hair follicles may subsequently use the follicular space as a path to disseminate to the skin surface and infect new hosts.
Skin wounding and photoaging are two events that may cause damaged keratinocytes to release growth factors promoting MCPyV infection. In such cases, the authors said that proliferation and migration of MCPyV-infected fibroblasts from the dermis to the above-lying wounded tissue or shedding layers of sunburned skin could represent another mode of transmission for MCPyV virions to depart from reservoir cells in the dermis and spread to new hosts.
“Despite our finding that MCPyV can effectively infect human dermal fibroblasts, the picture of MCPyV infection is far from complete. The identity of the natural host reservoir cells that maintain latent MCPyV infection in the human body remains elusive,” the authors wrote.
The incidence of MCC has tripled over the last few decades, underscoring the urgency for more effective therapies for this patient population. Treatment and management options for MCC depend on several factors including tumor location, stage, and patient comorbidities. Primary MCC is treated with wide local excision followed by radiation therapy and in addition to biopsy, a lymph node evaluation should be made in all patients with MCC. Here, clinically positive nodes should undergo fine needle aspiration/core biopsy, whereas those patients without clinically positive nodes should undergo sentinel lymph node biopsy (SLNB) for further evaluation.
Treatment for patients with nodal involvement includes nodal dissection or radiation therapy for clinically or radiologically apparent disease, and adjuvant nodal irradiation for negative nodes, microscopic disease or following nodal dissection for definitive disease. Combination therapies including chemotherapy, radiation therapy, surgery, and immunotherapy should be considered for those patients with loco-regional or more advanced disease. In addition to the dermatologist, those patients with metastatic MCC should ideally receive a multidisciplinary management approach including the oncologist, radiologist, and surgeon.
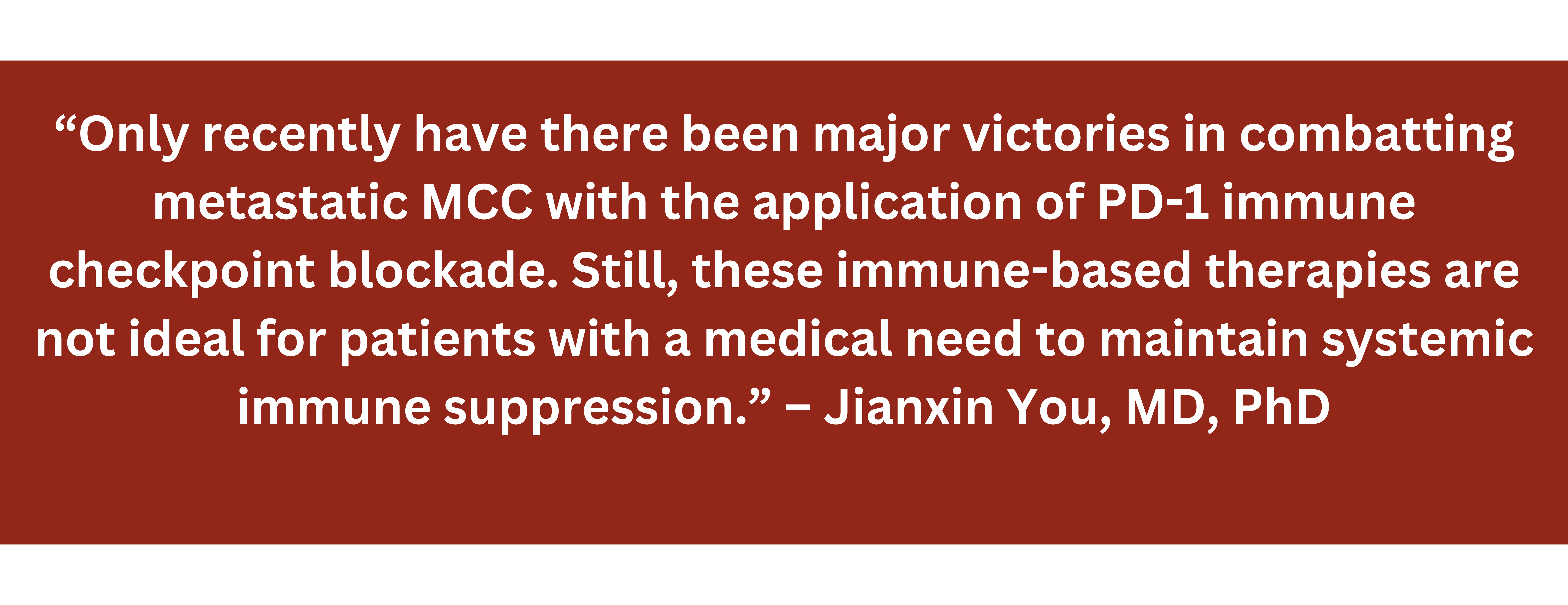
Recent breakthroughs in systemic therapy for advanced disease include immune checkpoint inhibitors targeting the programmed cell death 1 (PD-1) and programmed cell death ligand 1 (PD-L1) pathways. PD-L1 is often expressed on MCC tumor cells and peritumoral immune cells, while circulating MCPyV-specific T cells express PD-1. Blocking the interaction between PD-L1 and PD-1 is a key therapeutic target in the reactivation of the immune response for the treatment of many tumors, including MCC. Immune-based therapies such as FDA-approved pembrolizumab (Keytruda, Merck), and avelumab (Bavenico, EMD Serono, Inc/Pfizer), and nivolumab (Opdivo, Bristol Myers Squibb) still under investigation for advanced MCC have shown promising results in clinical trials. These novel anti-PD-1 and anti-PD-L1 antibodies function to restore active T cell response against the tumor.
“Only recently have there been major victories in combatting metastatic MCC with the application of PD-1 immune checkpoint blockade. Still, these immune-based therapies are not ideal for patients with a medical need to maintain systemic immune suppression,” the authors wrote.
Nevertheless, these human monoclonal antibodies that target PD-1 and PD-L1 and block the formation of the PD-1/PD-L1 complex resulting in the activation of T cell mediated immune responses look very promising and are providing much needed hope for a subset of MCC patients.
Reference
1. Yang JF, You J. Merkel cell polyomavirus and associated Merkel cell carcinoma. Tumour Virus Res. 2022 Jun;13:200232. doi: 10.1016/j.tvr.2021.200232.Epub 2021 Dec 15.
Disclosure
None relevant

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.