- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Melanoma tumor syndromes
Author(s):
Recognition of patients with hereditary melanoma is important not only because these individuals require careful surveillance for future primary melanomas, but also because they may be predisposed to multiple other types of malignancies because of their genetic mutation, says Hensin Tsao, M.D., Ph.D.

Recognition of patients with hereditary melanoma is important not only because these individuals require careful surveillance for future primary melanomas, but also because they may be predisposed to multiple other types of malignancies because of their genetic mutation, says Hensin Tsao, M.D., Ph.D., professor of dermatology and director, MGH Melanoma and Pigmented Lesion Center, Massachusetts General Hospital, Harvard Medical School, Boston.
“When we talk about familial melanoma today, we are moving away from a pure focus on patient susceptibility to develop multiple melanomas and towards awareness that cutaneous melanomas may be part of a mixed tumor syndrome,” Dr. Tsao says. Dr. Tsao spoke about melanoma tumor syndromes at the 2020 Dermatology Foundation Clinical Symposium.
“For some patients, the melanoma or another diagnostic melanocytic tumor may be a harbinger of risk for other internal malignancies. Early identification of these patients can be important so that they can be referred to other specialists as appropriate for additional cancer screenings,” he adds.
FAMM SYNDROME
Overall, only about 1% of patients with melanoma are thought to have a hereditary melanoma tumor syndrome. To date, a number of loci have been linked to hereditary melanoma, but the two most pronounced involve mutations in CDKN2A and BAP1 (BRCA1-associated Protein 1).
Overall, a mutation in CDKN2A is thought to occur in approximately 40% of hereditary melanomas. Associated with the familial atypical multiple mole-melanoma (FAMM) syndrome, the CDKN2A mutation leads to loss of function for producing the tumor suppressor protein p16.
Not all individuals with the mutation develop melanoma. Data on differences in risk based on geographic area of residence indicate that sun exposure, or other co-inherited factors, also plays a role.
“Among people with a CDKN2A mutation, the risk of melanoma is about >90% for those who live in Australia, about 76% for people living in the United States, but only 50% to 60% for people living in Northern England,” Dr. Tsao says.
Dermatologic follow-up for patients with a CDKN2A mutation involves two to four skin exams annually and stringent sun protection. The CDKN2A mutation also puts patients at risk for pancreatic cancer, and so these patients are also referred for consideration of routine pancreatic cancer screening by gastroenterologists.
BAP1 TUMOR SYNDROME
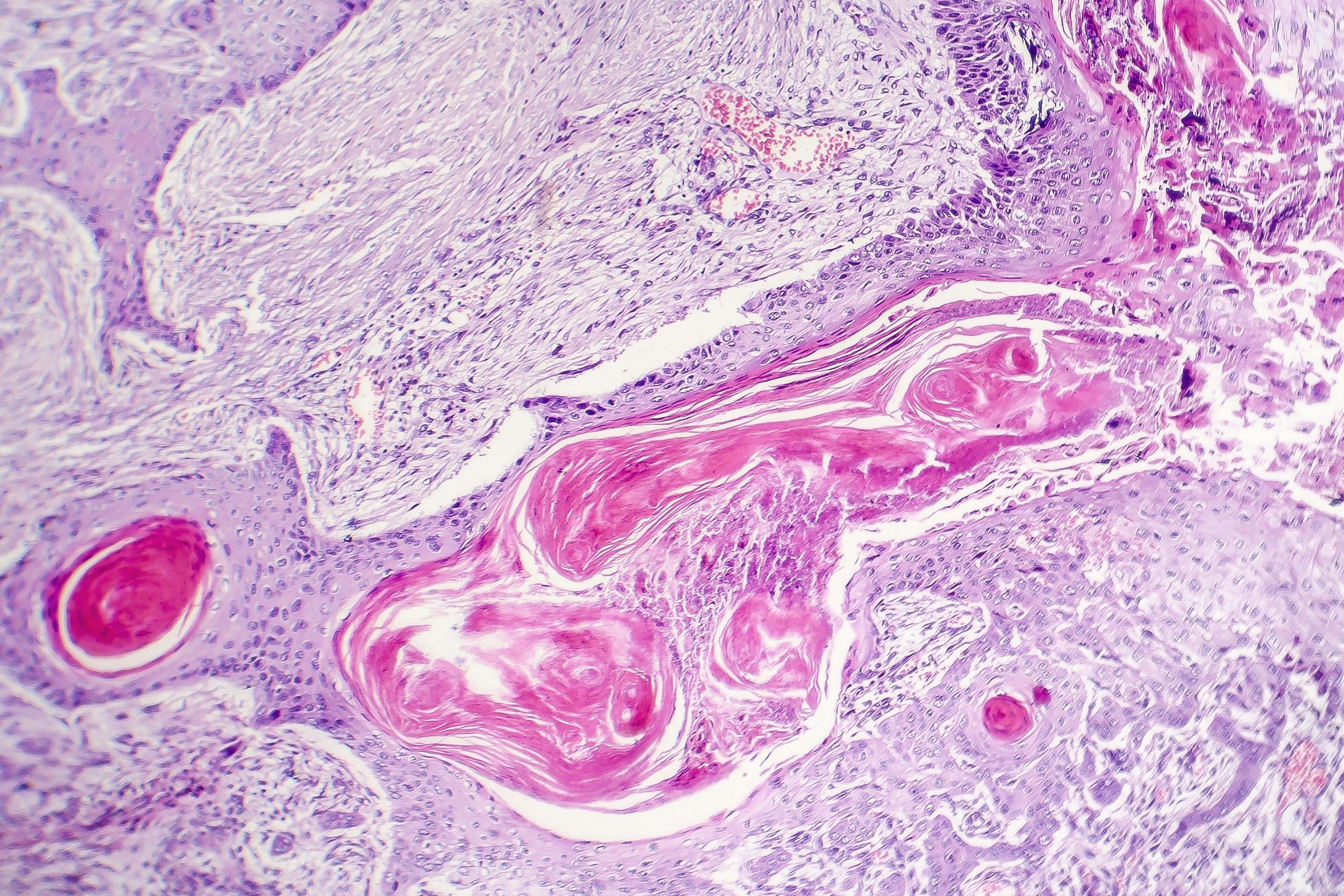
BAP1 tumor syndrome is far less common than FAMM, but it is associated with a longer list of organ system cancers than FAMM. Dr. Tsao says the mnemonic CRUMB can be used to remember the neoplasms that are part of the BAP1 syndrome: Cutaneous bapoms/melanoma, Renal cell cancer, Uveal melanoma, Meningioma andMesothelioma, Breast/ovarian carcinoma and Basal cell carcinoma mesothelioma, breast cancer. Lung, kidney and other cancers also occur. The underlying mutation also affects the function of a tumor suppressor gene. The BAP1 associated skin lesions are small, amelanotic, semi-translucent papules, plaques, or nodules.
Previously identified as nevoid melanomas, there are many terms for these lesions but they popularly are referred to as “BAPomas.”
Histologically, the BAPomas can have very atypical features that can simulate malignancy and are thus often re-excised with narrow margins; however, they do not appear to be highly aggressive.
“BAPomas usually do not progress like cutaneous melanomas, but BAP1 mutation carrier patients are also at risk for other skin cancers, particularly early onset basal cell carcinomas. Identifying BAPomas is important because these skin lesions may be one of the first markers of a germline BAP1 mutation,” Dr. Tsao says.
In addition to skin examinations, Dr. Tsao recommends patients undergo an annual ophthalmic exam to screen for uveal melanoma, and he refers these patients to other cancer specialists who decide on appropriate follow-up for other tumor types.
RARER MELANOMA TUMOR SYNDROMES
Recently discovered melanoma susceptibility genes also include a rare polymorphism in MITF (p.E318K), which occurs more often in people of European descent.
Patients with the germline MITF(E318K) variant often have atypical moles. Aside from melanoma, the association between the E318K variant and other cancers is somewhat controversial.
Dermatologic follow-up for these patients is generally scheduled once or twice a year.
“These patients are checked regularly because they have melanoma and atypical moles and not just because they carry the MITF mutation. The frequency of follow-up depends on how many melanomas and atypical moles they have,” he notes.
Dr. Tsao says he will also refer these patients to a kidney specialist who may follow them for renal cancer with a CT scan.
Most recently, germline mutations predisposing to melanoma have been reported in genes involved in telomere regulation, including TERT and members of the shelterin complex, such as POT1. Other types of cancers have also been observed in families harboring these mutations, but the number of patients is so rare that it is difficult to do proper genotype-phenotype correlation studies. Because they are so rare and only recently described, clinical these mutations have not yet been developed.
“With our current ability to sequence and read the genome, we will continue to uncover many more germline mutations conferring high risk for melanoma. Many of these will be ‘private mutations’ that occur in small families or even individuals, which is exciting for biology but less relevant for the general melanoma population. Therefore, it will be a challenge to determine their significance for patient follow-up,” Dr. Tsao says.
Disclosures:
Dr. Tsao has no relevant financial interests to disclose.

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.