- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
New device treats nonmelanoma skin cancer
Author(s):
A new energy-based device delivering ultrafast pulses of high amplitude electrical energy to nonthermally preferentially clear targeted cell rich lesions is proving to be a very useful treatment modality for a number of benign dermatologic lesions.
A new technology based on nano-pulse stimulation (NPS) appears to be effective for treating a growing list of benign dermatologic indications, and now it’s being investigated for nonmelanoma skin cancer, one expert says. With potentially fewer side effects, this technology has definitive advantages over traditional modalities that may make it an excellent treatment alternative in the future, says E. Victor Ross, M.D., Scripps Clinic Carmel Valley, Laser & Cosmetic Dermatology, San Diego, Calif., who spoke during the ODAC meeting in Orlando.
RELATED: Potential first-line treatment for advanced cutaneous squamous cell carcinoma
“Nano-pulse stimulation is an exciting new technology that likely has only touched the surface of its potential therapeutic utility in dermatology,” he says. “Beyond its proven efficacy in benign dermatologic lesions, this technology could potentially also prove useful in the treatment of nonmelanoma skin cancer such as basal cell carcinoma.”
The CellFX system (Pulse Biosciences) delivers ultrafast pulses of high amplitude electrical energy to non-thermally clear the targeted cells. The high amplitude energy pulses cause the creation of tiny pores which allow ions such as calcium to move within the cells of the target lesion. This shift triggers a cascade of significant changes and disruption of vital cellular organelle function, ultimately leading to regulated cell death (RCD), or apoptosis. Adjacent non-cellular tissues remain unaffected and the non-viable cells are gradually removed via the natural healing process. This foundation has been proven in the early basic science studies.
“The system uses a very high amplitude electrical field and very short pulses. It’s not radiofrequency, but direct current, so it doesn’t have a specific frequency in the sense of most other electromagnetic applications that are used in dermatology involving radiofrequency whether for aesthetic or non-aesthetic indications,” Dr. Ross says.
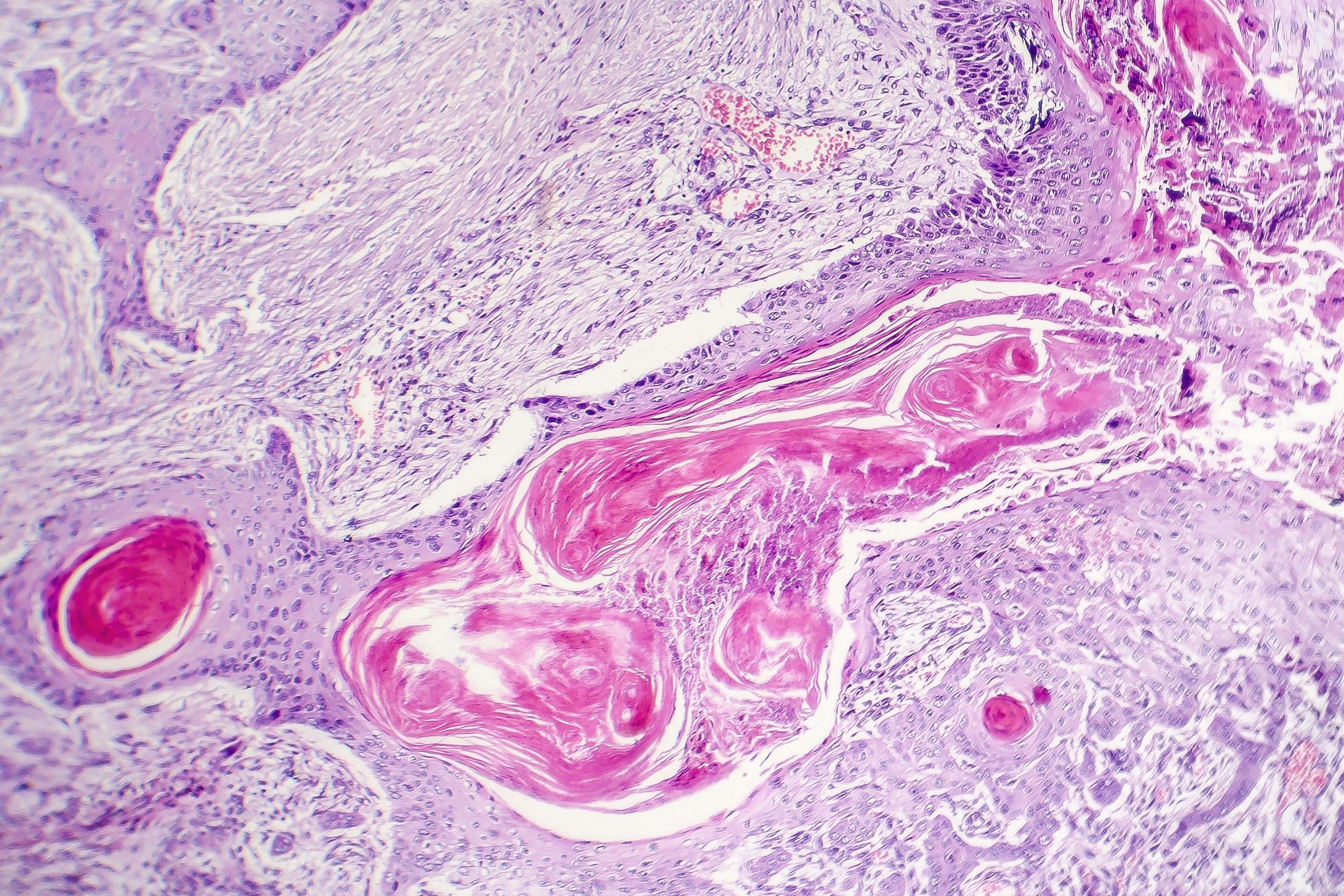
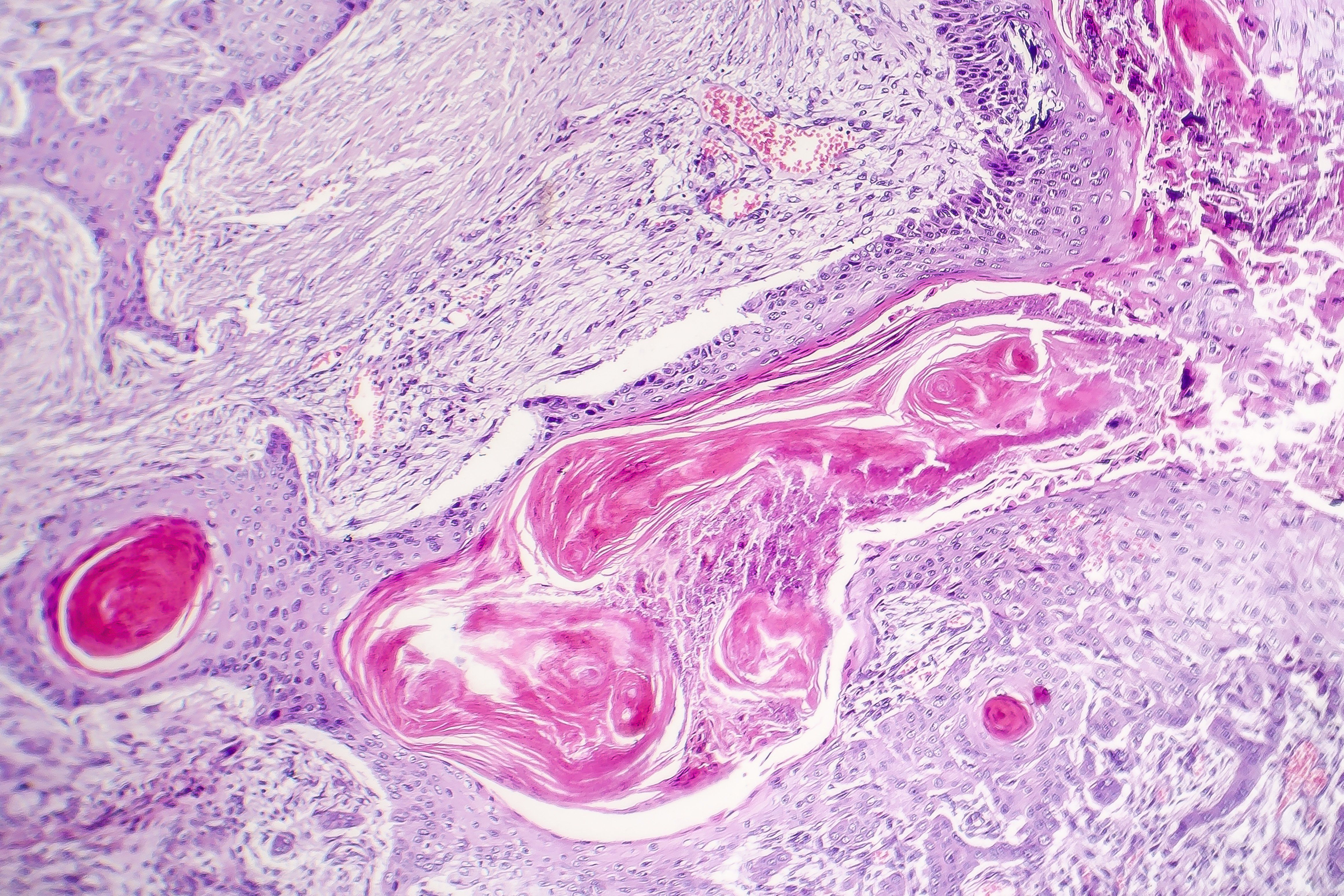
Researchers at Pulse Biosciences recently focused their efforts on evaluating the device’s efficacy in treating a number of benign dermatologic lesions including sebaceous hyperplasia, seborrheic keratosis, verrucae, and acne and have achieved excellent treatment outcomes. Interestingly, Dr. Ross says the NPS energy appears to be selective for cell rich lesions such as verrucae, seborrheic keratoses, sebaceous hyperplasia and acne, compared to cell poor lesions.
“The mechanism of action is not a thermal one. Typically, in dermatology with the exception of photochemistry and photodynamic therapy, most of our applications involve heat, meaning there is either the transfer of electrical energy to heat or optical pulses in the sense of laser devices into heat. This new approach is unique in that now we are applying electrical pulse direct current, not radiofrequency,” Dr. Ross says. “Even though the mechanism is not thermal, there is some pain involved during the procedure requiring local injectable anesthesia,” he adds.
RELATED: Targeted therapies for advanced basal cell carcinoma
Aside from not requiring sometimes cumbersome eye protection, a central working advantage associated with the system is that it is noninvasive in the sense that there is no plume during treatment. One of the key issues when treating warts with different lasers is that there is a plume that activates HPV virus and needs to be suctioned during treatment. Of note, Dr. Ross says that the CellFX treatment in warts is thought to have a broader immune-stimulatory effect where the immune system appears to be stimulated around the targeted lesion as has been witnessed in the disappearance of untreated warts in the vicinity of the target lesion.
On this premise, researchers have now also begun a trial in nonmelanoma skin cancer to examine the potential therapeutic benefit of this effect in basal cell carcinoma. The hope is that there may be a peripheral stimulatory effect that would remove some of the tumor that is not removed directly by the device itself. According to Dr. Ross, these dermatologic indications may only be the tip of the iceberg concerning the broad utility of this treatment approach in dermatology.
“This is a unique technology for dermatology, or even beyond dermatology. The initial results of the trials have been excellent, and the applications for this technology will only grow. The excitement is also that I think we are moving faster than I would have thought two to three years ago, and for cell rich lesions, this seems to be an interesting technology that may have even more uses down the line in dermatology,” Dr. Ross says.

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.