- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Case Report: Repigmentation of the Lips Using Ruxolitinib
Author(s):
Dive into a complex case report of a 29-year-old African American male patient with Fitzpatrick skin type V with a 6-month reported history of vitiligo on his lips.
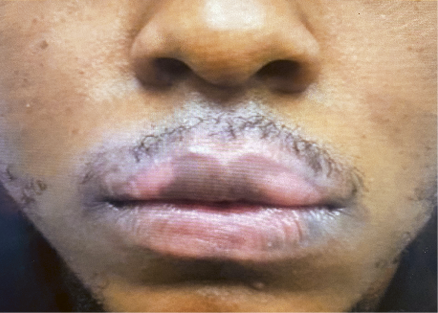
Figure 1. Patient photo before ruxolitinib. Photo courtesy of Malka Niknamfard, PA-C.
Vitiligo is perhaps one of the most universally recognizable skin conditions. Even those who don’t know the name of the condition can recognize its distinct appearance. Vitiligo is an autoimmune disease in which certain patches of skin lose their pigment, causing well-demarcated white spots on the skin. This occurs when melanocytes are attacked or destroyed and thus stop producing melanin.1,2 Although there is still much unknown, there are various theories surrounding the pathogenesis of vitiligo, the most common one being autoimmune destruction by an individual’s body. Vitiligo is the most common depigmentation disorder and affects 0.5% to 2.0% of the world’s population.3
In May 2023, I met with a 29-year-old African American male patient with Fitzpatrick skin type V with a 6-month reported history of vitiligo on his lips. His vitiligo started off as 1 small patch on his left lower lip, which he first thought nothing of. However, it began spreading throughout the rest of his lower lip as well as his right and left upper lip. He is otherwise healthy, with no other past medical history.
Prior to treating my patient, I made sure to set treatment and prognosis expectations. I explained that, unfortunately, there is no cure for vitiligo as of yet, and there are not many treatment modalities that have proven to be efficacious, especially within a short amount of time. We decided to do our best to try to stop its progression and eventually restore lost color back to the affected skin.
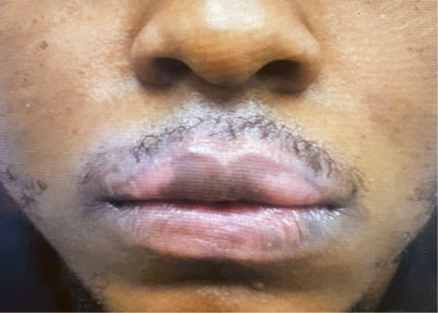
Figure 2. Patient photo after 4 months of ruxolitinib. Photo courtesy of Malka Niknamfard, PA-C.

After having tried multiple short-term courses of topical steroids and then switching to topical calcineurin inhibitors without improvement, my patient could not help but express his frustration. He hadn’t seen any results with the aforementioned medications and did not want to continue using them only to worry about the potential adverse effects of skin atrophy, telangiectasias, striae, and dermatitis. Although I recommended that he try phototherapy, he explained that he would not be able to take time off from work to attend sessions as frequently as 2 to 3 times a week.
After a few visits, I could tell my patient’s condition was continuing to cause him notable distress. He mentioned that he was single and the unsightly hypopigmented marks on his lips made it difficult to date. He said he felt as though all anyone was looking at when talking to him were the white marks on his lips. He was also constantly nervous and anxious about developing new spots on other parts of his face and body. My patient’s frustration was palpable, and I could see the emotional toll his condition took on his self-esteem and his quality of life. I even suggested that seeing a psychologist or joining a support group may be helpful.
A few weeks after not having seen results with the aforementioned medications, topical ruxolitinib (Opzelura; Incyte) became FDA-approved for the treatment of vitiligo in July 2023. I brought up the aforementioned patient to my pharmaceutical representative and told her I wanted to start my patient on ruxolitinib. However, when I told her that his vitiligo was localized to his lips, she explained that he unfortunately may not be the best candidate for treatment with ruxolitinib, as it works best on hair-bearing areas of the body because they contain hair follicles. After doing more research on the topic, I came to learn that melanocytes arise from the neural crest cells in the human body and then go through the skin dermis to differentiate, mature, and then reside in the hair follicles and epidermis. Hair follicles act as one of the main reservoirs for melanocytes, as melanocyte stem cells reside in the hair follicle bulge prior to maturation. Ruxolitinib works to essentially reduce T cell–mediated destruction of melanocytes to allow for melanocytes to slowly regenerate from hair follicles and lead to repigmentation of the skin over time. Thus, due to this dearth of melanocyte reservoir in lips, treating vitiligo in this area can be extremely difficult.4-6
Figure 3. Patient photo after 7 months of ruxolitinib. Photo courtesy of Malka Niknamfard, PA-C.
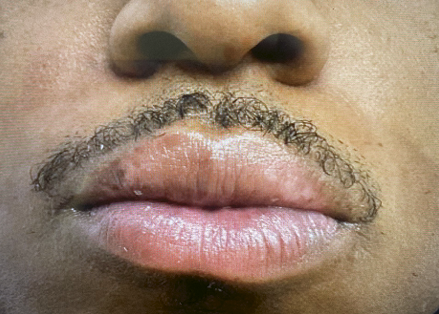
My patient and I mutually decided that trying ruxolitinib was worth a shot. I explained to him that it would take at least 6 months of consistent use to start seeing results, but that it would most likely take longer for him due to the location of his vitiligo. After seeing my patient back for a follow-up in October, 3 months after first prescribing him the ruxolitinib, I could not believe his results. There were signs of repigmentation significantly earlier than either one of us expected, and my patient was elated. I could sense his relief; the expression of happiness and gratitude on his face said it all. Figures 1, 2, and 3 demonstrate the patient’s progress prior to therapy, at month 4 of treatment, and at month 7 of treatment. I am extremely impressed with his results and am looking forward to seeing greater progression and improvement in his vitiligo over the coming months.
Malka Niknamfard, PA-C, is a physician assistant at Schweiger Dermatology Group in the Bronx, New York. She works with patients of all ages and diagnoses and treats a variety of different dermatological conditions.
References
1. Vitiligo. National Institute of Arthritis and Musculoskeletal and Skin Diseases. Updated October 2022. Accessed January 12, 2024. https://www.niams.nih.gov/health-topics/vitiligo
2. Vitiligo. Mayo Clinic. November 10, 2022. Accessed January 12, 2024. https://www.mayoclinic.org/diseases-conditions/vitiligo/symptoms-causes/syc-20355912
3. Joge RR, Kathane PU, Joshi SH. Vitiligo: a narrative review. Cureus. 2022;14(9):e29307. doi:10.7759/cureus.29307
4. Nishimura EK. Melanocyte stem cells: a melanocyte reservoir in hair follicles for hair and skin pigmentation. Pigment Cell Melanoma Res. 2011;24(3):401-410. doi:10.1111/j.1755-148X.2011.00855.x
5. Slominski A, Wortsman J, Plonka PM, Schallreuter KU, Paus R, Tobin DJ. Hair follicle pigmentation. J Invest Dermatol. 2005;124(1):13-21. doi:10.1111/j.0022-202X.2004.23528.x
6. Repigmentation reimagined. Incyte. Accessed January 12, 2024. https://www.opzelurahcp.com/vitiligo/
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.