- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
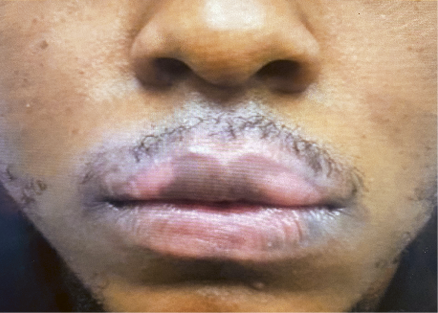
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Rare Disease Detection With AI: What Tools to Trust
Author(s):
Key Takeaways
- AI tools like OM1's Patient Finder enhance the identification and diagnosis of rare diseases by analyzing patient data patterns.
- Digital phenotyping technology helps detect early warning signals in patients' data, improving diagnosis and treatment of rare diseases.
From the February cover: Joseph Zabinski, PhD, MEM, and Stefan Weiss, MD, MBA, FAAD, share their expertise into AI’s capabilities in dermatology and specifically, rare diseases such as generalized pustular psoriasis.

“Rare Disease Day raises awareness for the 300 million people living with rare diseases around the world and their families and carers. Relatively common symptoms can hide underlying rare diseases, leading to misdiagnosis and [delayed] treatment,” writes the Rare Disease Day organization.1,2
Rare Disease Day has been observed globally every year on the last day of February since its creation in 2008. This year, Rare Disease Day is observed on February 29, and it is an opportunity to work toward increased awareness.
One of the emerging methods for further studying, analyzing, and detecting rare diseases and their characteristics is through artificial intelligence (AI).
Joseph Zabinski, PhD, MEM, the managing director of AI and personalized medicine at OM1, a real-world data, AI, and technology company with a focus on chronic diseases, and Stefan Weiss, MD, MBA, FAAD, the managing director of dermatology at OM1, exclusively share their expertise into AI’s capabilities in dermatology and specifically, rare diseases such as generalized pustular psoriasis. Zabinski and Weiss also address the common concern of with so many AI platforms available: How can clinicians trust AI’s data and learn from its insights?
Navigating Rare Dermatologic Diseases Using AI
By: Joseph Zabinski, PhD, MEM
Joseph Zabinski, PhD, MEM

There are a few issues that come up when we are trying to understand rare dermatologic diseases from the data access perspective and the patient journey perspective. The first is that patients with rare diseases tend to languish for long periods of time, sometimes going years without a diagnosis or having been misdiagnosed in another disease category. In both cases, this means we cannot access those patients’ data as far back in the record as we would like to so we can see where they began their disease states until they reach an accurate diagnosis. However, this is an area where having AI tools to help us look for undiagnosed or misdiagnosed patients can be helpful. Another point with respect to data accessibility is that in a lot of conditions that are more common, there are sometimes rare subtypes of the disease that may be hiding in large populations and in large datasets. Unless we have good tools that can pull out and isolate the patients who belong in those rare subtypes, they can get lost in the noise. It is not something you worry about so much with larger disease states where population average characteristics may be more important, but certainly, in the rare disease instance, it is quite important.
A Look at OM1’s Patient Finder
OM1’s Patient Finder is quite an exciting tool. It does what it says: find patients. It is built using our digital phenotyping AI technology, PhenOM. We can use PhenOM to understand patterning and signaling information in patients’ data histories, just like we might understand a patient’s genetic code by using genotyping, for example. If we can lay out the information in those patients’ histories and then use this digital phenotyping technology, we can ask, “What are some of the data elements that are unique for this patient and perhaps associated with a characteristic or an outcome of interest that that patient also has in their record?”
In the case of rare disease, we might collect a group of hundreds or thousands of patients with a rare disease and ask, “Using this technology, what data characteristics were present in this patient’s past before they reached a point of diagnosis that may have signaled that that’s where they were headed?” In other words, could we detect early warning signals? Patient Finder compresses those sets of signaling information into digital phenotypes; I think of them as fingerprints. Once we have the fingerprint for the disease, we can then compare new patients’ records to it.
This is where Patient Finder is powerful in deployment. We can use it to look at health system data and we can use it to look at other novel datasets, but once it understands that reference fingerprint, we have the ability to call out patients who are highly likely to match that fingerprint, meaning they are highly likely to have the condition that we’re looking for, even if they haven’t been diagnosed yet. By being able to call them out we can study them further, or, in clinical implementation, patients can be contacted, and if they consent, can proceed with diagnostic evaluation and potentially receive a diagnosis.
Improving Data Collection of Undiagnosed Conditions
Patient Finder works hand in hand with some of the other efforts that we work on at OM1 to gather data, improve the quality of data, and, ultimately, give us insight into where patients with rare diseases are, how they might more quickly be diagnosed, and then, if appropriate, be offered treatment for their condition. The first of those ways is to use Patient Finder’s ability to look at a dataset and ask, “Who are and how big is the population of patients hiding below the surface of this dataset who may have the condition that we are interested in finding?” It is often the case, at least if we are talking about a rare disease with dedicated diagnostic coding, that we can find some patients in a dataset. However, we also have a hypothesis that there are others, as I describe them, beneath the surface who have similar clinical characteristics in their background, but who are not yet labeled with a code that lets us easily filter the dataset to find them.
Patient Finder can look at a dataset and say, “In addition to the few thousand people that you found, here are another 500 who are highly likely to also belong in that population.” That capability can do useful things such as giving us a better sense of true disease prevalence. Sometimes this is useful in a clinical trial context. Recruitment is a significant challenge in trials, and the ability to point to places where patients who may have been missed are concentrated can be helpful for recruitment efforts and figuring out how to optimize site selection.
The other way that Patient Finder helps with understanding and improving data gathering and processing for rare diseases is in the context of more proactive data gathering. This is another concept we spend a lot of time on at OM1: constructing digital registries, which can be interesting in the rare disease context. Patient Finder can help us by saying, “As the patient moves along in their journey, it is possible that early on in their journey, they have some indications that they may be on the path to a certain outcome, a certain progression, or a certain diagnosis.” We may not be sure yet, but Patient Finder can give us a sense as they progress of how their likelihood is changing. Is their path converging toward something of interest to us with respect to the clinical outcome? Or is it bending away from that? The ability of Patient Finder to say, “At this moment in time, for this data stream I am looking at, these patients look similar to the target group that I care about” is quite a powerful application in enhancing data availability for patients with rare diseases.
AI’s Role in Improving the Lives of Patients With Rare Diseases
tampatra/AdobeStock

There are a couple of things that I have learned in my career by working with people impacted by rare diseases and trying to understand them better to develop treatments. First is that each rare disease is unique. Of course, there are relationships among various rare diseases, but with somewhere close to 7000 rare diseases, they remain remarkably different from one another. This is true clinically and is also just as true at the data level when we are trying to understand what is going on with patients in the data. It is true with AI as well; just because you have a model that does well in one rare disease does not mean that the same thing will work well in another rare disease. That is why our whole digital phenotyping approach is designed to go one level deeper than just point-solution modeling. It is designed to say, “We can reflect what is true about the patient and their data characteristics.” Then we can use that greater flexibility to understand different rare diseases through pattern matching, again just like we might first understand a patient’s genetics, and then look for specific disease-associated mutations. I do think that both AI and data can be quite helpful with better understanding rare disease patients’ trajectories and ultimately getting them better treatment if we can be more precise in distinguishing them from everyone else.
This is one of my personal areas of focus, this notion that rare disease patients get lost so often in larger disease populations. They may have certain symptoms of a rare disease and go to see their primary care provider, have some testing done, and eventually receive negative results, so they go back to their primary care provider, or they go from specialist to specialist without answers. That kind of pinballing around can take years from patients’ lives. If we can reach a nice visibility into what a patient journey looks like and use AI to point out patients who are somewhere along that journey, we can be much more impactful. We are being much more impactful in clearing up some of that long-term dragging out of the process and getting patients at least to the point of being treated by a specialist and having access to available treatments much more quickly.
Gaining Clinicians’ Trust of AI Tools
AI is certainly a buzzword, and it’s not always positive. If we read the popular press headlines these days, most are about problems with AI. They are about privacy violations, instances where AI has made incorrect predictions, and those have resulted in bad real-world consequences. This is one reason we are much more conservative in health care with respect to using AI than in some other industries. That said, there is a real path toward trust with AI tools. If we can establish that trust, AI tools can accomplish impressive improvements all over the world as it is today.
The first thing I focus on is contextualizing what AI can and cannot do. In a clinical treatment context, AI is a helper tool. It is not a decision maker that replaces clinicians. It is something that should be able to provide some additional insight and additional personalized vision for providers at the point of care to the patient sitting in front of them. AI can say things such as, “This patient looks like they are at an elevated risk of having XYZ condition, or they may be more likely to respond to this treatment or more likely to have a negative reaction.” You may want to consider those findings in your conversation with the patient. That is the appropriate application for AI tools today.
The other consideration is, and this is something we have built into Patient Finder and the underlying PhenOM technology, the ability to explain why AI says what it does. Many people have experimented with ChatGPT and other large language model tools. It is amazing the kinds of answers these tools generate, but it is mysterious to think about how they produce these answers. And I do not think it is obvious, even in many cases for experts, how the model came up with the output it produced in any specific instance. We focus on explainability for our tools like Patient Finder, by which we mean the ability to sit down with clinical experts who know the disease but do not know the AI part and say, “These are the factors that pointed the model in this direction.”
It is not the same thing as saying there is a smoking gun, that if the patient had a twitching left eyelid and a rash on their thumb, then they have this very specific condition. It is not that simple or straightforward. That is another myth that gets caught up in the AI hype. However, when you can have a conversation and say, “This is what this patient’s phenotypic profile looks like. This is how it is different from others, and that is why the model pulled this patient out of the broader pool,” I found that to be quite an effective way of building trust with clinicians helping them see how AI can integrate into their practice.
Looking Ahead
I keep hearing that 2024 is the year that AI grows up. We will see if that is true; we can check in again in January 2025. But I think and I hope that there is an opportunity now, perhaps through the popularization of AI, for it to have a mature impact in the coming months and years, especially in areas that are often neglected, such as rare diseases.
Joseph Zabinski, PhD, MEM, is the managing director of artificial intelligence and personalized medicine at OM1.
Revolutionizing GPP Recognition Through Data Collection
By: Stefan Weiss, MD, MBA, FAAD
Stefan Weiss, MD, MBA, FAAD

The American Academy of Dermatology’s (AAD) DataDerm is the largest single registry of dermatology patients in the country, which forms the foundation for any data analysis that can be done within dermatology at OM1. OM1’s Patient Finder, in its purest form, is the ability to identify individuals who may suffer from a disease but lack awareness that they carry it. As such, it can identify an individual who may not present with the disease until later in life. Patient Finder can also identify individuals who may perform better or worse on a certain therapeutic in terms of either efficacy or safety. As it relates to generalized pustular psoriasis (GPP), deploying Patient Finder was an opportunity to focus on individuals who have a rare disease, GPP, that often goes undiagnosed or misdiagnosed for a very long time.
For background on GPP, these individuals tend to present with pustules all over their body. As many do not know to see a dermatologist, they will often find themselves in urgent care or in the emergency department, which could spiral into a hospital admission and extensive use of antibiotics. Identifying in advance those individuals who may carry GPP offers the opportunity to be more proactive about care delivery, either connect with a dermatologist proactively or at least recognizing that should a flare occur, informing the rendering provider that neither hospitalization nor extensive antibiotic use is necessary. The partnership between OM1’s Patient Finder and AAD’s DataDerm for GPP is really an opportunity to drive improvements in patient care.
Future Opportunities for Patient Finder
There are some dermatologic diseases that we all can recognize from 100 yards away. However, many are hard to distinguish, especially for the non-dermatologist. Recognizing the individuals who are more likely to carry and present with a certain disease can be extremely helpful. The best example of another dermatologic condition for which Patient Finder would be useful is hidradenitis suppurativa (HS), a disease where cysts form under the breasts, in the groin, or under the arms. When these cysts form as a one-off, individuals often find themselves in a primary care office. Women quite frequently go to their gynecology clinic. Many patients visit urgent care to have the cysts lanced. However, cyst removal is not going to treat the underlying condition. If we can identify in advance those individuals as suffering from HS, we are better able to connect them to the health care system for appropriate treatment.
GPP Treatment and Diagnosis Challenges
One of the main challenges of diagnosing and treating GPP is finding physicians who recognize the disease. GPP is a rare disease and like all rare diseases, it is quite infrequently seen by even by the specialists who may treat it. By leveraging large datasets to identify carriers of the disease, those individuals can be better managed.
Rare diseases, dermatologic or otherwise, are rare, and therefore hard to recognize, diagnose, and treat. If we can use AI for identification, we can improve the care that those people receive.
Addressing AI as a Buzzword
In medicine, there is hesitancy around AI because of the concern that the “machine” will take over from the human.
Because AI sees patterns more rapidly, it has been highly leveraged in pathology and radiology. Despite the visual nature of dermatology, there remains the need in dermatology to understand the whole patient. A single picture of a red itchy plaque on the elbow may be eczema, it may be psoriasis, it may be fungal-related. In the end it can be the manifestation of many different diseases. It is challenging for the machine to make that determination without having greater context. Thus, AI is not there to take over the role of the clinician, but rather to help and improve patient care.
If AI can determine that patient X would do better on drug A than drug B in terms of either safety or efficacy, then it is a valuable tool in finding the right patient the right drug at the right time. That is the way AI should always be regarded within the clinical arena.
Stefan Weiss, MD, MBA, FAAD, is the managing director of dermatology at OM1.
Reference
1. Rare disease day. Rare Disease Day. Accessed January 17, 2024. https://www.rarediseaseday.org/
2. What is a rare disease. Rare Disease Day. Accessed January 17, 2024. https://www.rarediseaseday.org/what-is-a-rare-disease/
Share your experiences with treating rare dermatologic diseases by emailing DTEditor@mmhgroup.com.
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.