- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
News
Article
Dermatology Times
Communication Is Key in Atopic Dermatitis Treatment
Author(s):
A discussion among roundtable participants revolved around the importance of effective communication, the impact of prolonged use of topical steroids, and the need for trust building in recommending novel treatment options.

“Long gone are the days of just walking in a room for 30 seconds, saying, ‘Here’s your prescription,’ and so on and leave. Now, we have to have patients appreciate that we’re on the same level so that patients can trust us,” said Omar Noor, MD, FAAD, of Rao Dermatology in Atlantic Highlands, New Jersey.
Atopic dermatitis (AD) often poses challenges in terms of treatment options and patient communication. Noor moderated a recent Dermatology Times Case-Based Roundtable Meeting, “Deciphering Challenging Scenarios: Practical Insights Into Atopic Dermatitis Management.” He led a discussion among local dermatology clinicians about approaches to complex AD cases. Communication was key in a case involving a 28-year-old African American woman with AD. The discussion among roundtable participants revolved around the importance of effective communication, the impact of prolonged use of topical steroids, and the need for trust building in recommending novel treatment options.
The Importance of Communication
Noor emphasized the critical role of communication in dermatology, particularly when discussing treatment options with patients. Gone are the days of brief interactions; now, patients need to be part of a dialogue that helps them understand not just what they are prescribed but also why and how to use it. This shift requires dermatologists to build rapport and instill confidence in patients, especially when introducing newer and novel treatment options.
He said, “You can feel the confidence and you have to make sure the patient feels that confidence to push through because they may feel the improvement early on, but they have to continue with the treatment and to make sure that patients feel comfortable with utilizing it over a longer period of time.”
Building Trust in Recommendations
One of the key challenges highlighted in the discussion was the issue of trust, particularly when patients have been on topical corticosteroids for extended periods. “When we tell them about a newer, more novel option, they may not trust us to give them that option,” Noor explained. “We have to earn that trust, and to earn that trust, we have to be able to communicate with them.”
Noor stressed the need for dermatology clinicians to earn patients’ trust by effectively communicating the reasons behind treatment recommendations. He mentioned the use of strategies like combining topical corticosteroids with topical ruxolitinib (Opzelura) to address concerns about rebound effects and facilitating a smoother transition.
“Depending on the individual, depending on our rapport with that individual, making sure that we develop that trust with the patient, because if we’re going to talk about changing an algorithm, changing the paradigm, changing the way someone has treated their disease for years, they have to trust us, and so we have to be confident in recommending that medication,” he added.
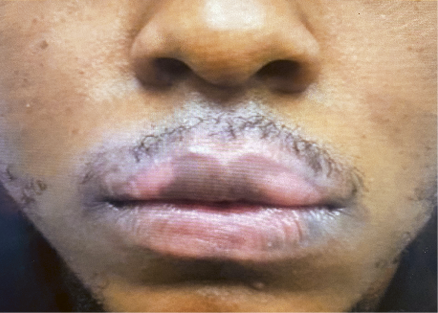
Addressing Hyperpigmentation Concerns
The case discussed involved hypopigmentation resulting from the overuse of topical steroids. Noor and the group of roundtable participants acknowledged the prevalence of this issue and the importance of tailoring treatment to individual skin types and ethnicities. The discussion touched upon the cautious use of stronger topical corticosteroids in patients with a higher risk of hypopigmentation.
Optimizing Treatment in Sensitive Areas
The conversation delved into the utilization of topical ruxolitinib or steroid-sparing agents, particularly in more sensitive areas. The consensus was that these agents could be applied not only in sensitive areas but also over larger body surfaces. However, questions arose about the duration of use, with considerations for reevaluation if improvement is not observed within a specified time frame.
Biopsy Considerations
Noor emphasized the importance of considering biopsy in cases where patients do not respond to treatment as expected. While AD is not often biopsied, he highlighted the need to rule out other potential diagnoses. This cautious approach ensures that dermatologists do not overlook alternative explanations for a lack of treatment response.
“If someone is not responding [to a treatment] the way that you anticipate, take a step back and maybe biopsy that patient. We want to make sure that we’re not missing other diagnoses, whether it’s connective tissue disease, or even mycosis fungoides or cutaneous T-cell lymphoma,” he explained.
Tailoring Treatment to Skin of Color
The interview shed light on the nuances of treating AD in individuals with darker Fitzpatrick skin types. The roundtable group discussed the avoidance of stronger topical corticosteroids in certain ethnicities due to concerns about hyperpigmentation. Tailoring treatment plans based on individual characteristics and establishing trust in the patient-physician relationship were recurring themes.
Ensuring Access to Medication
“We have to feel confident in access, and everyone [in the roundtable] felt the same way. Everyone felt that we need to feel confident they can get the medication,” Noor said.
The conversation concluded with a discussion on the practical aspect of ensuring patients have access to prescribed medications. Noor and the group emphasized the need for dermatologists to facilitate medication access. Strategies such as collaborating with specialty pharmacies and providing detailed notes for prior authorization were highlighted as effective ways to streamline the process and make treatments more accessible to patients.
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.