- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
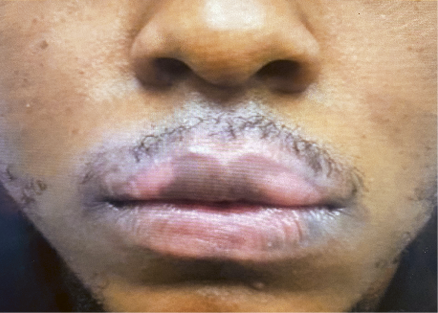
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
News
Article
Dermatology Times
From Conjunctivitis to Itch Control: RAD Research to Keep an Eye on
Learn more about dupilumab-induced conjunctivitis rates and misconceptions, the thriving long-term efficacy of dupilumab over 3 years, and unraveling the itch-flare dynamic in abrocitinib treatment.
Several late-breaking research sessions were presented during the recent Revolutionizing Atopic Dermatitis Virtual Conference, showcasing new data in atopic dermatitis (AD) treatment. Here are a few highlights in case you missed it.
Examining Rates of Conjunctivitis in Dupilumab-Treated Patients
Matthew Zirwas, MD, of Dermatologists of Greater Columbus in Columbus, Ohio, did a deep dive on dupilumab (Dupixent)-induced conjunctivitis. Dupilumab, known for inhibiting both IL-4 and IL-13, has been associated with conjunctivitis as a comorbidity in AD. The presentation aimed to address questions about the frequency and clinical significance of this adverse event, particularly in patients with AD.
Zirwas highlighted the challenge of differentiating between conjunctivitis cases that are dupilumab-induced and those that are part of the underlying AD disease process. The study he discussed involved analyzing data from randomized, double-blinded, and placebo-controlled trials conducted under regulatory conditions. These trials included diverse age groups, from preschoolers to adults, and varied in duration from 16 to 52 weeks.
Contrary to misconceptions from postmarketing studies reporting conjunctivitis rates as high as 20%, Zirwas clarified that the vast majority of conjunctivitis cases occurred within the first 16 weeks of treatment. In 16-week monotherapy trials, there was a notable disparity between placebo (2%) and dupilumab-treated (9.3%) conjunctivitis cases. Even in 52-week trials, the increase in conjunctivitis cases was marginal, emphasizing that clinically meaningful cases tend to occur early in the treatment.
Persistent conjunctivitis cases throughout the trials occasionally led to participant dropout, with approximately 2% of dupilumab-treated patients experiencing clinically meaningful conjunctivitis, which could potentially limit therapy. Zirwas noted that this pattern was not observed in people treated with dupilumab for other indications.1
Thriving Through 3 Years: Dupilumab’s Long-Term Efficacy
Benjamin Lockshin, MD, of U.S. Dermatology Partners in Rockville, Maryland, presented a study aimed to assess the long-term real-world effectiveness and safety of dupilumab over a 3-year period using data from the PROSE registry (NCT03428646). The population included patients aged 12 years and olderwith moderate to severe AD who initiated real-world dupilumab treatment as per approved prescribing information.
All enrolled patients received their first administration of commercially available dupilumab at the baseline visit, with no restrictions on dosing changes or concomitant medication use postbaseline. The study presented data from the safety analysis set, with an interim analysis cutoff date of June 15, 2022. The mean duration of dupilumab treatment was 23.1 months.
Results showed sustained improvement in clinical signs, symptoms, and quality of life for up to 3 years in patients with moderate to severe AD after initiating dupilumab treatment. The safety findings were consistent with the known dupilumab safety profile. Adverse events included conjunctivitis, COVID-19, AD, eczema, dry eye, and urticaria, with deaths reported in 2 cases related to events like congestive cardiac failure and gastric cancer.
The study observed positive and sustained outcomes in terms of clinical improvement and safety in patients with moderate to severe AD over a 3-year period following the initiation of dupilumab treatment, as evidenced by the interim analysis from the PROSE registry. The reported safety findings aligned with the established safety profile of dupilumab.2
Beyond the Surface: Unraveling the Itch-Flare Dynamic in Abrocitinib Treatment
Martin Steinhoff, adjunct professor at Hamad Bin Khalifa University in Qatar, presented a study focused on patients with moderate to severe AD treated with abrocitinib (Cibinqo), an oral Janus kinase (JAK) 1–selective inhibitor, analyzing data from the phase 3 JADE REGIMEN trial. AD often exhibits fluctuating severity, with periods of remission interrupted by flares. Abrocitinib, approved for adults and adolescents in the US and United Kingdom and adults in the European Union, showed initial efficacy in the trial, with patients receiving continued treatment or placebo during the maintenance period.3
The post hoc analysis aimed to assess itch response as a predictor of flares in patients who experienced flares during the 40-week maintenance period. The study included patients aged 12 and above with moderate to severe AD and a recent history of inadequate response or intolerance to topical AD treatment.
Results indicated that after a successful initial response with abrocitinib, patients who did not experience flares maintained stable mean itch scores (PSAAD itch NRS approximately 2.0). In contrast, among those who experienced flares, 76% to 92% showed worsening of itch from 2 weeks before flare onset to the day of flare. Mean itch scores were approximately 2.5-fold greater than baseline 2 weeks before the flare and approximately 4-fold greater on the day of flare.
The study suggests that monitoring itch may serve as a valuable predictor of flare onset in patients with moderate to severe AD treated with abrocitinib.
References
- Zirwas M. Conjunctivitis adverse events in dupilumab clinical trials. Late-breaking research presented at: Revolutionizing Atopic Dermatitis Virtual Conference; December 10, 2023.
- Lockshin B. Real-world effectiveness of dupilumab in adult and adolescent patients with atopic dermatitis: 3-year data from the PROSE registry. Late-breaking research presented at: Revolutionizing Atopic Dermatitis Virtual Conference; December 10, 2023.
- Steinhoff M. Worsening of itch before flaring in patients with moderate-to-severe atopic dermatitis treated with abrocitinib: a post hoc analysis of the phase 3 JADE REGIMEN trial. Late-breaking research presented at: Revolutionizing Atopic Dermatitis Virtual Conference; December 10, 2023.
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.