- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
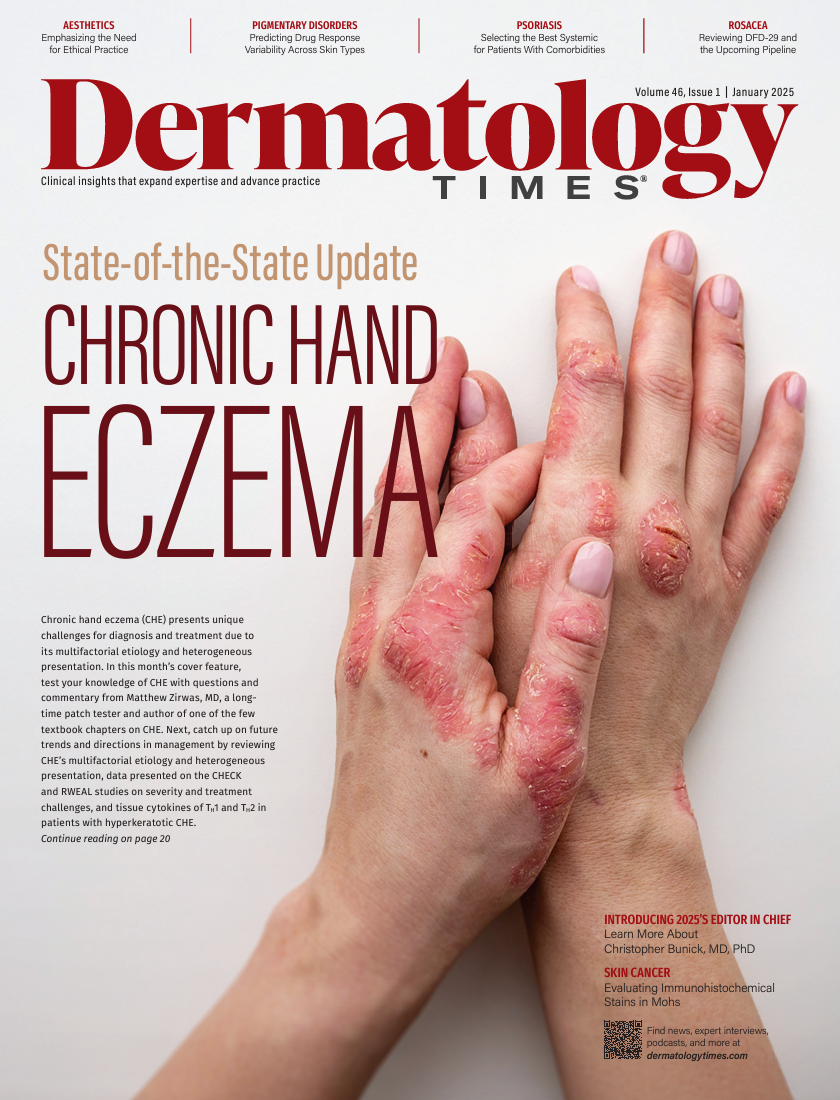
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
News
Article
Dermatology Times
Identifying Ancestry-Specific Clinical End Points in Diverse Trials
Author(s):
Key Takeaways
- Historical exclusion of diverse populations in clinical trials leads to biased therapeutic outcomes and safety profiles.
- Ancestry-specific clinical endpoints are crucial for addressing disparities in drug response and safety.
Researchers are advancing inclusive trials through ancestry-specific endpoints, focusing on skin tone variability, melanin's role, and precision drug modeling.
Image Credit: © Elle Bramble/Cultura Creative -stock.adobe.com

The drive for inclusivity in clinical trials has never been more urgent. Historically, the clinical research landscape has often excluded sufficient representation from diverse populations, leading to potential biases in therapeutic outcomes and safety profiles.1 This limitation has direct consequences for clinical care, particularly when the genetic, biochemical, and physiological nuances of different ancestral backgrounds are overlooked.1 The integration of ancestry-specific clinical end points into research frameworks is essential to address these disparities effectively. To streamline the transition to diverse clinical trials, it is crucial to identify ancestry-specific clinical end points.
A recent article highlights the need for assessing risk related to skin tone variations and offers a scalable, cost-effective approach to predicting drug response variability across population groups.2 By leveraging cell-based assays, biochemical screening, and computational modeling, this strategy aims to account for chemical interactions with melanin.2 Such variability is also relevant in industries such as cosmetics and agriculture, where melanin-related toxicity can influence safety assessments, an area that is currently underexplored in regulatory frameworks.2
The Importance of Risk Assessment for Skin Tone Variability
One significant dimension of patient diversity is skin tone. Variability in skin pigmentation not only influences aesthetic characteristics but also affects drug absorption, metabolism, and dermal reactivity to treatments.3 For example, individuals with darker skin tones may exhibit different barrier functions due to variations in ceramide content and stratum corneum structure, affecting topical drug absorption and systemic response.3 Identifying these differences at an early stage is crucial in tailoring clinical trials that are inclusive of the broad spectrum of skin tones.
The current lack of targeted end points that consider skin tone variability can lead to suboptimal therapeutic recommendations and adverse effects in underrepresented populations. Thus, refining risk assessment protocols to incorporate skin tone–specific factors can bridge gaps in drug response predictions and enhance overall patient safety.
Leveraging Cell-Based Assays for Precision in Drug Response Prediction
Cell-based assays have emerged as potential tools in assessing drug response variability across different population groups. By cultivating cells with genetic backgrounds representative of diverse ancestries, researchers can evaluate how distinct phenotypic traits impact cellular reactions to specific drugs.4 This approach has the advantage of providing direct insight into the interaction between drug compounds and cellular mechanisms that might differ by ancestral background.
These assays can simulate the behavior of skin cells with varying melanin content, elucidating how pigmentation can alter drug permeation and efficacy. For instance, one study demonstrated that topical corticosteroids exhibited varied anti-inflammatory responses based on melanin concentration in skin cell models.5 Such findings underscore the necessity of including a wide range of skin tones in drug response studies.
Biochemical Screening: A Scalable Approach for Drug Testing
Biochemical screening complements cell-based assays by providing a high-throughput method to detect biomarkers predictive of drug responses across different populations.2 By isolating specific biochemical signatures, researchers can identify pathways that are more active or subdued in certain ancestries, allowing for more targeted treatment protocols.
This methodology is particularly cost-effective, as it can be integrated into existing research infrastructures and scaled to assess large numbers of compounds. Screening for enzymes involved in drug metabolism, such as cytochrome P450 variants, has been shown to reveal significant interethnic variability in drug clearance and adverse effect profiles.6 By adapting these screenings to include melanin-associated markers and related proteins, trials can better predict responses and adverse effects in patients with diverse skin tones.
Computational Modeling: Advancing Predictive Capabilities
The rise of computational modeling has further enriched the landscape of precision medicine. These models integrate genetic, phenotypic, and environmental data to simulate how drugs interact within varied biological systems. Machine learning algorithms can process complex data sets that include skin tone variability, predicting drug responses and adverse reactions more accurately.7
For example, incorporating skin tone data into computational simulations of topical corticosteroid application can project differences in absorption rates and efficacy, guiding formulation adjustments to optimize treatment outcomes for all skin types.8 This approach also enables researchers to preemptively identify subgroups that might be at higher risk for certain adverse effects, refining the safety profile of drugs before they enter broad clinical use.
Toward Ancestry-Specific Clinical End Points
Identifying specific clinical end points that reflect genetic and phenotypic diversity is critical for advancing inclusivity in trials. These end points might include biomarkers for inflammatory responses that vary by skin tone, pigmentation-related drug interactions, and differential risks for adverse effects associated with darker skin types.9
Furthermore, collaboration with dermatologists and geneticists is warranted to establish comprehensive clinical trial guidelines that integrate skin tone and ancestral background as key factors. Standardizing these practices will enhance the external validity of trial outcomes and ensure that therapies are optimized for diverse patient groups.
Conclusion
The transition to inclusive clinical trials that incorporate ancestry-specific clinical end points is essential for advancing equity in health care. Risk assessment protocols that account for skin tone differences, supported by cell-based assays, biochemical screening, and computational modeling, offer a robust framework for enhancing trial inclusivity. This approach not only improves predictive accuracy for drug responses but also fosters a more equitable landscape for therapeutic development and application. By applying these strategies, researchers can create scalable and cost-effective models that accommodate the genetic and phenotypic diversity of human populations, ultimately improving treatment outcomes and safety for all patients.
Isabella J. Tan is a third-year medical student at Rutgers Robert Wood Johnson Medical School in New Brunswick, New Jersey.
References
- Khozin S, Coravos A. Decentralized trials in the age of real-world evidence and inclusivity in clinical investigations. Clin Pharmacol Ther. 2019;106(1):25-27. doi:10.1002/cpt.1441
- Zaaijer S, Groen SC. Implementing differentially pigmented skin models for predicting drug response variability across human ancestries. Hum Genomics. 2024;18(1):113. doi:10.1186/s40246-024-00677-7
- Salminen AT, Manga P, Camacho L. Race, pigmentation, and the human skin barrier—considerations for dermal absorption studies. Front Toxicol. 2023;5:1271833. doi:10.3389/ftox.2023.1271833
- Xia F, Allen J, Balaprakash P, et al. A cross-study analysis of drug response prediction in cancer cell lines. Brief Bioinform. 2022;23(1):bbab356. doi:10.1093/bib/bbab356
- Brazzini B, Pimpinelli N. New and established topical corticosteroids in dermatology: clinical pharmacology and therapeutic use. Am J Clin Dermatol. 2002;3(1):47-58. doi:10.2165/00128071-200203010-00005
- McGraw J, Waller D. Cytochrome P450 variations in different ethnic populations. Expert Opin Drug Metab Toxicol. 2012;8(3):371-382. doi:10.1517/17425255.2012.657626
- Chan S, Reddy V, Myers B, Thibodeaux Q, Brownstone N, Liao W. Machine learning in dermatology: current applications, opportunities, and limitations. Dermatol Ther (Heidelb). 2020;10(3):365-386. doi:10.1007/s13555-020-00372-0
- Lundborg M, Wennberg CL, Narangifard A, Lindahl E, Norlén L. Predicting drug permeability through skin using molecular dynamics simulation. J Control Release. 2018;283:269-279. doi:10.1016/j.jconrel.2018.05.026
- Markiewicz E, Karaman-Jurukovska N, Mammone T, Idowu OC. Post-inflammatory hyperpigmentation in dark skin: molecular mechanism and skincare implications. Clin Cosmet Investig Dermatol. 2022;15:2555-2565. doi:10.2147/CCID.S385162
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.






















