- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
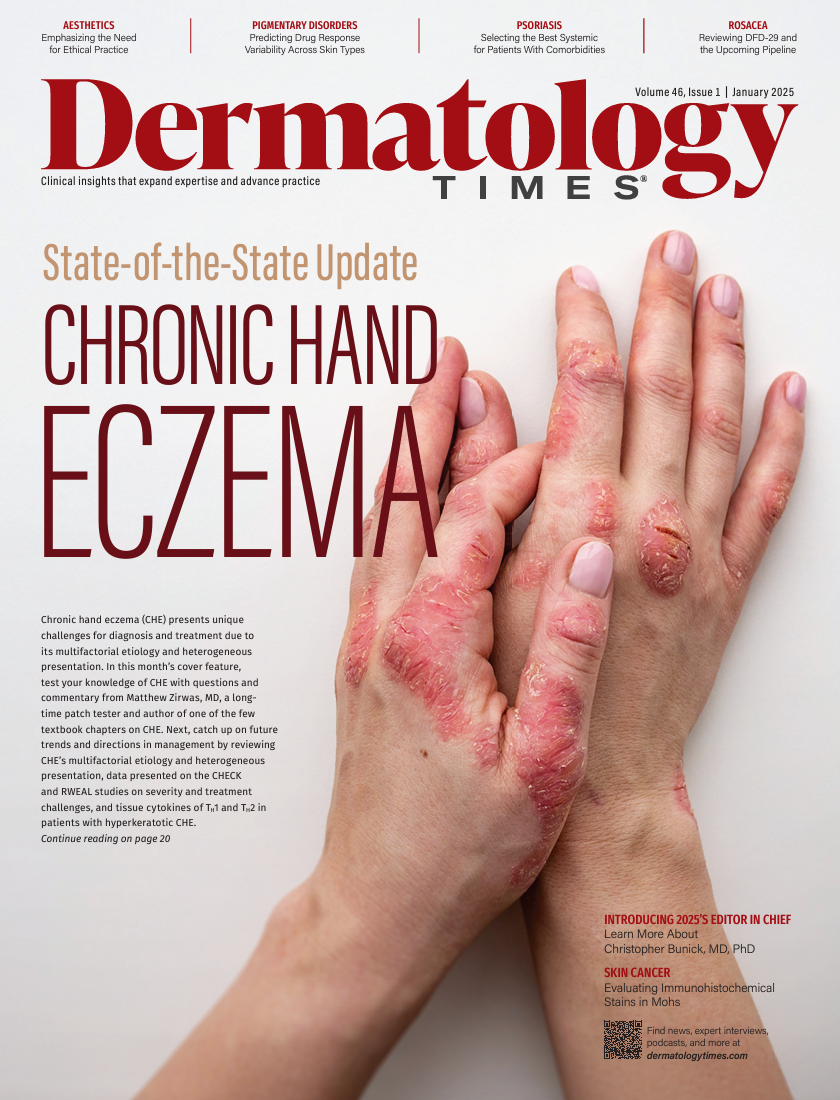
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
News
Article
Dermatology Times
The Role of Immunohistochemical Stains in Mohs Surgery
Author(s):
Key Takeaways
- Immunohistochemistry (IHC) enhances diagnostic accuracy in Mohs micrographic surgery (MMS), especially for poorly differentiated tumors and melanoma.
- IHC stains like PanCK, SOX10, and Ber-EP4 improve tumor identification and margin assessment, reducing recurrence rates in skin cancer treatment.
Explore the role of immunohistochemical stains in enhancing diagnostic accuracy during Mohs surgery, aiding treatment of challenging skin cancers.
Hard of hearing and flashing a large smile, he sat down on the soft blue clinic chair after driving for 2 hours to come for Mohs micrographic surgery (MMS) treatment. He was an 80-year-old male patient referred for Mohs for a rapidly growing, poorly differentiated squamous cell carcinoma (SCC) on his scalp. It started as a small pink papule and over the past 2 months had grown to a large, crusted plaque. The aggressive nature, large size, and bizarre histological features on pathology had revealed poorly differentiated SCC cells. Sometimes the poor differentiation of a tumor can make it more difficult to identify cells on standard hematoxylin and eosin (H&E) staining.
Image Credit: © steheap - stock.adobe.com

During Mohs, the patient went 2 stages and on the final slide there was a focal area of cells that was suspicious for dense inflammation vs residual tumor. Given the original poorly defined cell morphology, definitive identification was challenging. To confirm accurate diagnosis and avoid unnecessary removal of more tissue, we used a pan cytokeratin (PanCK) immunohistochemical stain. We used this stain to clearly highlight the presence of epithelial tumor cells, confirming that there were no SCC cells and that the final margins were clear of tumor. This case employed immunohistochemistry (IHC) and its critical role in aiding decision-making during complex Mohs procedures.
There is a growing popularity of using IHC stains in MMS, especially for challenging cases involving poorly differentiated tumors and melanoma. In this article, we will explore the applications, advantages, limitations, and considerations of important IHC stains in Mohs surgery. IHC can enhance diagnostic accuracy and lead to better long-term patient outcomes.
Understanding Immunohistochemistry in Mohs Surgery
The gold standard for surgical skin cancer removal, MMS uses H&E staining on fresh frozen sections to examine the deep and lateral margins of tissue. It is successful at decreasing recurrence rates for skin cancer because it evaluates 100% of the tissue margins while using accurate mapping.1,2 Sometimes H&E can be difficult to interpret, so IHC staining is used to supplement and verify the standard stains. The technique of IHC staining uses antibodies to detect specific antigens within cells.3,4 By visualizing these antigen-antibody interactions, pathologists can identify neoplastic cells with enhanced precision. IHC is especially useful when conventional H&E staining is insufficient, as in cases of poorly differentiated tumors or when distinguishing neoplastic cells from reactive or normal tissues is challenging.
Important IHC Stains in Mohs Surgery
One of the most widely used IHC stains is MART-1 (melanoma antigen recognized by T cells 1) or Melan-A.5,6 It targets a melanocyte-specific protein, highlighting melanocytes in the epidermis and dermis that are found in melanoma in situ and invasive forms. This stain is very sensitivefor melanocytes but not specific for malignant melanocytes. MART-1 can stain benign melanocytic lesions like nevi, and it has limited utility in spindle cell and desmoplastic melanoma.7 It can be used in a 1-hour protocol to process and stain melanomas.1
SOX10 is an IHC stain with greater sensitivity that targets a nuclear transcription factor in melanocytes and neural crest cells.1 It is helpful for detecting desmoplastic and spindle cell melanomas on MMS slides, especially because these may go undetected on H&E and with MART-1. The melanoma nuclei are stained with the SOX10 stain and highlight areas of melanoma involvement.8 Unfortunately, a limitation of SOX10 is that it can stain benign neural elements in scar tissue, which could lead to overdiagnosis.
There is a 98% to 99% cure rate for MMS in the treatment of basal cell carcinoma (BCC) and SCC.9 For high-risk BCC, the stain Ber-EP4 targets the epithelial cell adhesion molecule. It is very effective in differentiating BCC from benign follicular proliferation or folliculocentric basaloid hyperplasia.10 Also, there are tumor specimens that can have a basosquamous component. The Ber-EP4 can help decipher whether the tumor is BCC vs SCC vs sebaceous tumor in origin. Some physicians also use Ber-EP4 to confirm clear margins when the BCC is morpheaform or infiltrative, especially in the setting of dense inflammation on the pathology slides. However, the limitation for this stain is its weak or absent staining in poorly differentiated BCC subtypes.
One of our favorite stains to use is PanCK, which targets a variety of cytokeratin proteins in epithelial cells.1 It most often is used to detect SCC and its poorly differentiated forms. It is highly sensitive for epithelial tumors and helpful in identifying subtle or ambiguous residual tumor cells. A limitation of this IHC stain is that it may be less specific and some benign epithelial areas including sebaceous glands may become highlighted. We tend to implement this stain most often for poorly differentiated SCC.
Dermatofibrosarcoma protuberans (DFSP) is a rare, malignant fibrohistiocytic tumor with a high rate of recurrence after surgical excision.11 Historically, a wide local excision with margins of 2.0 to 2.5 cm conferred recurrence rates, up to 75% in the head and neck areas. MMS has significantly lower recurrence rates up to 7% over a 5-year period. CD34 is an antibody IHC stain that targets glycoproteins found in vascular endothelial and spindle cells. CD34 distinguishes DFSP tumor cells from fibrotic scar or reactive tissue. Also, CD34 tends to stain DFSP tumor cells, well unlike in its benign counterpart, the dermatofibroma.1 A limitation is that CD34 can also stain endothelial cells and perivascular fibroblasts, which requires discretion by the surgeon.
Finally, another popular IHC stain is cytokeratin 7 (CK7), which targets glandular and transitional epithelium cytokeratin proteins.12
We use CK7 for diagnosing extramammary Paget disease (EMPD) and clearing the MMS margins for this noncontiguous disease. A limitation of CK7 is that it cannot differentiate between CK7 expressing metastatic adenocarcinomas vs primary EMPD.
Comprehensive Applications and Considerations
Pros of Using IHC Stains in Mohs Surgery
IHC stains enhance diagnostic precision in MMS as a supplement to H&E staining. It helps to further clearly visualize malignant tumor cells in cases that may be difficult to interpret. IHC can ensure accurate margin assessment, thereby minimizing unnecessary removal of tissue while confirming complete tumor excision. Also, IHC can provide increased confidence in complex cases by resolving ambiguous histological findings. The presence of dense inflammatory infiltrates can obscure the detection of residual tumor cells and leave tumor behind.13,14 IHC can be used to highlight tumor within the inflammation, leading to decreased risk of tumor recurrence.
Cons of Using IHC Stains in Mohs Surgery
Despite the benefits of its use, IHC staining has some drawbacks. First, because IHC was initially designed for use in permanent pathology section and not frozen sections, there can be issues with the stability of antigens on frozen.16 Second, IHC does increase procedural costs because of the purchase of necessary equipment and reagents. Third, working with IHC also requires histotechnology and Mohs surgeon specialized training. Not all Mohs fellowships teach fellows how to use IHC, and some practicing surgeons have never used IHC. Fourth, there are extra steps in processing and interpreting IHC slides that can extend surgical time. The incubation time for each stain varies and sometimes can take up to 2 hours to process. Finally, the risk of nonspecific staining or background artifact poses a risk of misinterpretation. There can be less specificity with some antigens that also are found in normal tissue structures.
Despite the drawbacks, IHC can help MMS to more accurately treat high-risk tumors. It may be most helpful to selectively use it for the most complex cases where routine H&E staining is not clear. IHC as a supplement to MMS helps to identify tumor cells with challenging pathology. Incorporation of more IHC in MMS is the advance our field needs to decrease recurrence rates for patients. MMS surgeons can optimize IHC into workflow optimization through strategic scheduling of patients and streamlining laboratory processes to minimize time delays.
Conclusion
Immunohistochemical stains are a significant advancement in Mohs surgery. They provide the Mohs surgeon greater precision for tumor identification and margin assessment. Dermatologic surgeons can decrease skin cancer recurrence and minimize unnecessary removal of skin by using IHC stains such as PanCK or SOX10. Although IHC requires more resources and training, it is the next best step in cutaneous oncology for setting the gold standard for complex skin cancer treatment.
References
- Sroa N, Campbell S, Ravitskiy L. Immunohistochemistry in mohs micrographic surgery: a review of the literature. J Clin Aesthet Dermatol. 2009;2(7):37-42.
- Rapini RP. Comparison of methods for checking surgical margins. J Am Acad Dermatol. 1990;23(2 pt 1):288-294. doi:10.1016/0190-9622(90)70212-z
- Polak JM, Van Noorden S. Introduction to Immunocytochemistry. 2nd ed. Garland Science; 1997.
- Robinson JK. Current histologic preparation methods for Mohs micrographic surgery. Dermatol Surg. 2001;27(6):555-560. doi:10.1046/j.1524-4725.2001.00339.x
- Jimenez FJ, Grichnik JM, Buchanan MD, Clark RE. Immunohistochemical techniques in Mohs micrographic surgery: their potential use in the detection of neoplastic cells masked by inflammation. J Am Acad Dermatol. 1995;32(1):89-94. doi:10.1016/0190-9622(95)90190-6.
- Dawn ME, Dawn AG, Miller SJ. Mohs surgery for the treatment of melanoma in situ: a review. Dermatol Surg. 2007;33(4):395-402. doi:10.1111/j.1524-4725.2007.33085.x
- Plaza JA, Bonneau P, Prieto V, et al. Desmoplastic melanoma: an updated immunohistochemical analysis of 40 cases with a proposal for an additional panel of stains for diagnosis. J Cutan Pathol. 2016;43(4):313-323. doi:10.1111/cup.12654
- Albero-González R, Marti-Marti I, Alós L, et al. Margin control of lentigo maligna with SOX10-frozen section immunostaining: a case series. Australas J Dermatol. 2023;64(4):544-546. doi:10.1111/ajd.14132
- Krunic AL, Garrod DR, Viehman GE, Madani S, Buchanan MD, Clark RE. The use of antidesmoglein stains in Mohs micrographic surgery: a potential aid for the differentiation of basal cell carcinoma from horizontal sections of the hair follicle and folliculocentric basaloid proliferation. Dermatol Surg. 1997;23(6):463-468.
- Sunjaya AP, Sunjaya AF, Tan ST. The use of BEREP4 immunohistochemistry staining for detection of basal cell carcinoma. J Skin Cancer. 2017;2017:2692604. doi:10.1155/2017/2692604
- Parker TL, Zitelli JA. Surgical margins for excision of dermatofibrosarcoma protuberans. J Am Acad Dermatol. 1995;32(2 pt 1):233-236. doi:10.1016/0190-9622(95)90132-9
- Smith KJ, Tuur S, Corvette D, Lupton GP, Skelton HG. Cytokeratin 7 staining in mammary and extramammary Paget’s disease. Mod Pathol. 1997;10(11):1069-1074.
- Agnetta V, Williamson S, Bisbee E, et al. A retrospective review of histopathologic features associated with increased risk of recurrence of non-melanoma skin cancer after Mohs micrographic surgery. J Clin Aesthet Dermatol. 2022;15(1):27-29.
- Kim SW, Roh J, Park CS. Immunohistochemistry for pathologists: protocols, pitfalls, and tips. J Pathol Transl Med. 2016;50(6):411-418. doi:10.4132/jptm.2016.08.08
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.



























