- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
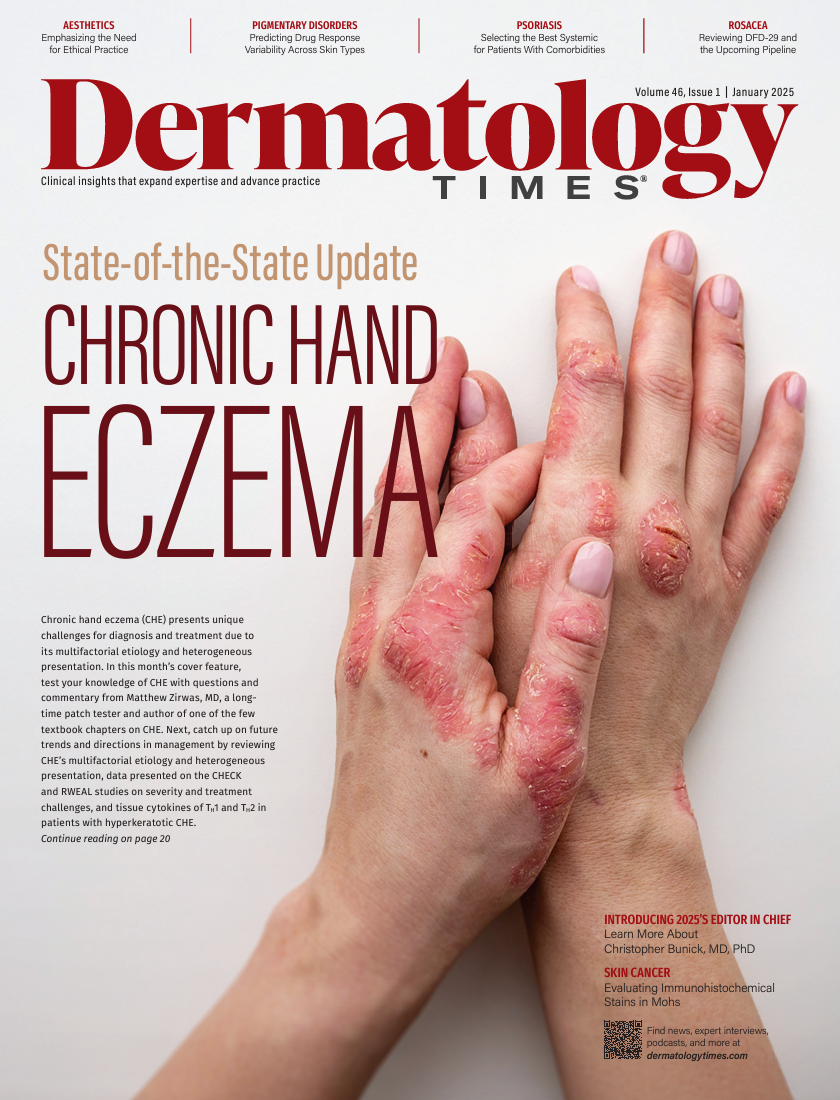
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
News
Article
Dermatology Times
The Intersection of Ethics, Aesthetics, and Patient Expectations in Dermatology
Author(s):
Key Takeaways
- Aesthetic medicine requires balancing ethical standards with patient expectations, often influenced by social media and unattainable ideals.
- Core ethical principles include respect for autonomy, beneficence, nonmaleficence, justice, and equality, guiding practitioners in aesthetic medicine.
Balancing ethics, aesthetics, and patient expectations is crucial in dermatology to ensure safe, responsible, and ethical care.
In today’s rapidly evolving field of aesthetic medicine, the convergence of ethics, aesthetics, and patient expectations presents a complex landscape for practitioners. The modern aesthetic industry faces unique challenges due to its elective nature, often centered on enhancing or altering a patient’s appearance based on personal desires. This discretional aspect can sometimes clash with ethical standards, primarily when patients’ expectations are influenced by unattainable external influences.
Image Credit: © BillionPhotos.com - stock.adobe.com

Practitioners must navigate these intersections with care, ensuring that they provide services that are not only safe and effective but also ethically sound. A delicate balance is required in aesthetic medicine, which converges on examining the ethical standards that guide the industry, the impact of patient expectations, and practical strategies for managing these expectations responsibly.
An Overview of Ethical Standards in Aesthetics
In the 1980s, 4 principles were established as the core commitments for ethical issues in the health care industry as a whole. These are as follows:
- Respect for patient autonomy
- Hippocratic concepts of beneficence and nonmaleficence (what is often thought of as “do no harm”)
- Justice and equality
- Concern for the scope of application1
The medical field, and especially aesthetic medicine, is not the same as it was in the 1980s, but these core principles remain. As this sector has progressed over the past 40 years, many treatments being offered today could not have been conceived of when that definition was written. Therefore, there is a lack of agreement in the medical field on where and by whom medical aesthetic treatments should be performed. This can mean that procedures are performed by people who do not have a medical degree and are not bound by the Canadian Medical Association Code of Ethics and Professionalism2 or the American Medical Association (AMA) Code of Ethics,3 which rigorously outline the virtues, fundamental commitments, and professional responsibilities of an ethical physician. Dermatologists in the US are also guided by the American Academy of Dermatology (AAD), which outlines similar standards.
Any doctors who employ professionals without a medical degree still have an ethical obligation to train their staff members properly and to thoroughly vet potential employees before hiring to ensure their qualifications. As a doctor, you are responsible for the practitioners working under you. Should they cross an ethical line, responsibility will ultimately fall on you and your practice to some degree.
Aesthetics are also unique in the medical field, as treatments are often voluntary. They aim to enhance or change the patient’s appearance according to the patient’s wishes. However, some medical aesthetic treatments can also be prescribed by physicians for specific conditions, such as migraines, excessive sweating, and temporomandibular joint dysfunction.
Maintaining strong ethical principles is also legally important for medical aesthetics providers, as ethical issues can quickly become legal ones. If a provider isn’t following ethical guidelines, they may find themselves in a medical malpractice suit that could have been avoided.
Adjacent to patient expectations for results is the understanding that information about a medical practitioner and their services will be accurate and readily accessible. A lawsuit against Allure Esthetic, a major plastic surgery provider in Seattle, Washington, was filed in 2022, and unethically misleading patients was the crux of the case. The clinic allegedly forced patients to sign nondisclosure agreements, bribed them to remove negative reviews, and threatened legal action if they refused. Employees were ordered to post fake positive reviews, and patient rebates were illegally claimed by the clinic. The attorney general, Bob Ferguson, noted the need to stop deceptive practices and hold the clinic and its practitioners accountable for misleading consumers in this way.4 Overall, the importance of maintaining ethical standards is underscored by how easily ethical breaches can turn into real legal issues.
While the elective nature of aesthetic treatments offers patients the opportunity to enhance their appearance, it also demands a high level of ethical vigilance to ensure that these procedures are conducted safely and responsibly.
Case Study: Navigating Patient Expectations
When a patient wants a voluntary medical aesthetic treatment, there are times when their expectations and desires are not compatible with what can be provided ethically and safely. Patients may have seen something on social media and thought that it was possible to replicate it on their bodies, such as getting the same amount of lip filler as an influencer has said they received. Educating the patient on how a more appropriate amount will achieve their needs may be required to maintain an ethical service.
Figure

Social media use before and after the COVID-19 lockdowns has also changed people’s perceptions of cosmetic procedures, including the number of people who follow accounts related to cosmetic procedures, who have thought about getting a cosmetic procedure, who have talked to their physician about a cosmetic procedure, and who believe that one will improve their self-esteem (Figure).5
In the past few years, we have seen an uptick in patients coming in with photos of what they want their facial features to look like. We reiterate to patients that no 2 faces are identical and that it’s almost impossible to put someone else’s lips on theirs. Furthermore, social media posts are often edited with filters and other changes to make people seem more refined, flawless, and attractive. This further distorts the perceptions and aesthetic desires of clients.
Tips for Managing Patient Expectations
As an aesthetic medical practitioner, there will be times you must deny service to patients due to ethical conflicts. There are many reasons why, including the health and safety of the patient and your own capacity to perform the treatment to their specifications.
When this happens, there are ways to communicate with the client to highlight the conflicts and ensure that they understand why you are denying the treatment—either temporarily or entirely.
- Respect for autonomy: Listen to the patient’s concerns and address those directly. Understanding what they want from treatment and what their goals are can inform how you proceed with the assessment.
- Hippocratic concepts: If the patient is experiencing a temporary contraindication to treatment, such as a medical condition that will pass, create a long-term care plan for them to return for treatment at a later date.
- Justice and equality: Educate the client on the service they are requesting and what its limitations are, including the specific reasons why you may need to deny it.
- The scope of application:
- When applicable, provide suitable alternative treatments to the patient. Many common concerns, such as addressing wrinkles and fine lines, have a multitude of treatments that can target them, all of which have different contraindications and may be suitable for different patients. When creating treatment plans, always ensure alternatives are offered only after confirming differing treatments are compatible with the patient’s medical history.
- If the patient has unrealistic expectations for the treatment they’re seeking, show them examples of people who have similar goals and the actual results they have achieved through that treatment to help them visualize a successful outcome. All examples should be from treatments you have performed personally and shared only with the consent of the individual who received treatment.
Conclusion and Resources
The intersection of ethics, aesthetics, and patient expectations in the field of aesthetic medicine is a delicate and complex terrain that requires thoughtful navigation by practitioners. While the elective nature of aesthetic treatments offers patients the opportunity to enhance their appearance, it also demands a high level of ethical vigilance to ensure that these procedures are conducted safely and responsibly. Practitioners must balance respecting patient autonomy with their core ethical principles, even as they manage the heightened expectations of patients.
As a doctor bound to the ethical standards of your medical association, it is also vital that you train and oversee your staff. You must also hold them to comparable standards.
There are different resources available to you and your clinicians to be proactive in ethical training and to seek counsel when issues arise. Examples are as follows:
- Complete training through your regulatory association, such as the AMA EdHub Ethics Training Course (https://edhub.ama-assn.org/
collections/42108/ethics), the AAD Training for Dermatologists (https://www.aad.org), or the Canadian Association of Aesthetic Medicine Training Program (https://caam.ca/training-program). - Contact an ethics consultation service as soon as a situation that presents a question of ethics arises.
- Contact your medical indemnity service provider for counsel when facing a malpractice suit.
By complying with established ethical standards, educating patients, and employing clear communication strategies, aesthetic medical professionals can uphold the integrity of their practice while meeting the evolving needs and desires of their patients. Ultimately, maintaining this balance not only fosters trust and satisfaction but also reinforces the credibility and ethical standing of the aesthetic industry as a whole.
Samuel Hetz, MD, MSc

Samuel Hetz, MD, MSc, is the medical director of Dermapure Wellington Village (previously Concept Medical), a physician-led medical aesthetic practice located in Ontario, Canada. Hetz completed his residency in family medicine at the University of Ottawa, followed by a fellowship in primary care skin conditions and office-based surgical procedures.
References
- da Prato EB, Cartier H, Margara A, et al. The ethical foundations of patient-centered care in aesthetic medicine. Philos Ethics Humanit Med. 2024;19(1):1. doi:10.1186/s13010-024-00151-1
- CMA Code of Ethics and Professionalism. Canadian Medical Association. 2018. Accessed July 10, 2024. https://policybase.cma.ca/viewer?file=%2Fmedia%2FPolicyPDF%2FPD19-03.pdf
- Code of Medical Ethics. American Medical Association. 2017. Accessed August 22, 2024. https://code-medical-ethics.ama-assn.org/
- AG Ferguson files lawsuit against Seattle-based plastic surgery clinic for bribing, threatening patients to falsely inflate its online ratings. News release. Washington State Office of the Attorney General. December 29, 2022. Accessed August 22, 2024. https://www.atg.wa.gov/news/news-releases/ag-ferguson-files-lawsuit-against-seattle-based-plastic-surgery-clinic-bribing
- Khan IF, De La Garza H, Lazar M, Kennedy KF, Vashi NA. Effects of the COVID-19 pandemic on patient social media use and acceptance of cosmetic procedures. J Clin Aesthet Dermatol. 2024;17(3):42-47.
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.


























