- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
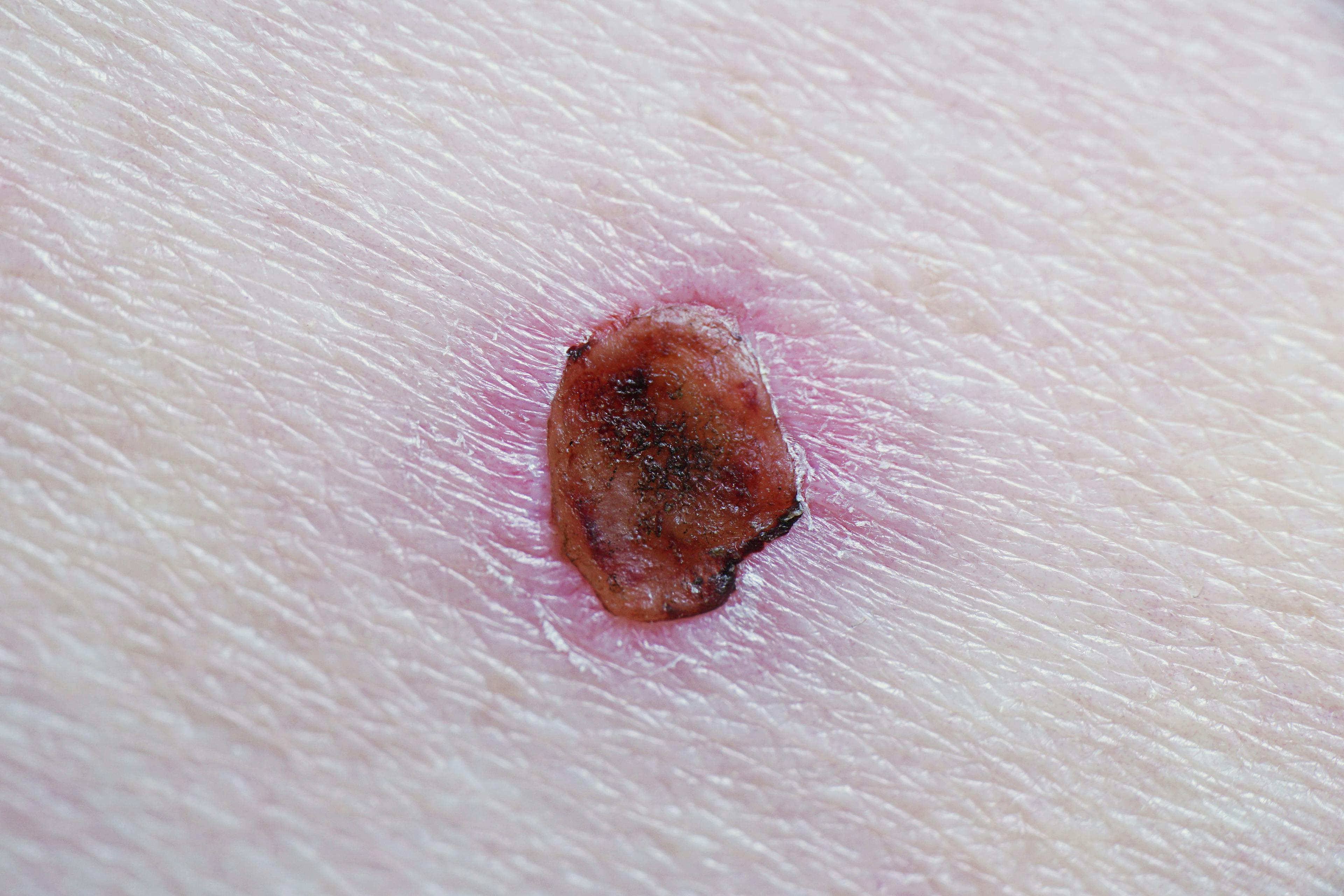
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
A Look at the Rise in Adult Acne in Women
Author(s):
Understanding the main causes and staying current on recommendations and treatments will help reduce patient rates of the condition.
Adult acne in women has increased 10% worldwide over the past 10 years, according to a 2022 review of adult acne conducted by Brigitte Dreno, MD, PhD, head of the Department of Dermatology at Nantes University Hospital in France, and colleagues. The review was published in the International Journal of Dermatology.1
“In adults, acne has serious consequences, including a psychological impact, low self-esteem, social isolation, and depression,” the authors wrote. The condition affects more than 640 million people across the globe, with the biggest risk factor being heredity.1 However, there are factors under patient control, such as diet, that can reduce acne risk.
Treatment approaches vary by gender, and newer treatments are in the pipeline, including skin microbiome modulation, which would be helpful in reducing antibiotic use and preventing microbial resistance.1
Anais Aurora Badia, MD, DO, an adult and pediatric dermatologist and founder of the Florida Skin Center, now part of Advanced Dermatology and Cosmetic Surgery in Fort Myers and Lehigh Acres, Florida, spoke with Dermatology Times® on the increasing rates of adult acne and how to treat it.
Factors Contributing to Adult Acne
Badia said that adult acne and adolescent acne share similar causes and that acne is mostly caused by sebum production, inflammation, and bacteria. “Stress, hormones and diet can increase inflammation,” she said. “When our stress levels rise, we produce higher levels of acne-causing androgens, which can stimulate oil glands and hair follicles that contribute to acne.”
In addition to stress—which has been considerably higher these past few years due to the pandemic—Badia said that masks worn to protect against COVID-19 increased acne rates because they trap dirt and bacteria on the skin, which contributes to an increase of the acne-causing bacteria Propionibacterium acnes.
Badia also noted gender differences in acne prevalence. “Increased hormone levels contribute to acne in both men and women. However, the types of hormones causing acne are different for each,” she explained. “Women tend to see more fluctuations in hormones than men due to medications, menstrual cycles, and menopause,” which is why women get more acne than men.2
Diet also plays a role in developing acne. “Some small studies have shown a link between dairy consumption causing an increased risk for acne,” Badia said. “Other studies have linked high glycemic index foods to acne [because] these foods spike our blood sugars rapidly, causing inflammation, which in turn leads to an increase in acne.” The review by Dreno and colleagues also found that milk, sugar, sugary drinks, and fatty foods were associated with acne in adults.1
Badia added that skin and hair products can also cause acne. She said that dermatologists should advise patients to read labels and look for products that say noncomedogenic or oil free.
“It is also important they be advised to use products with physical sunscreens, such as zinc oxide or titanium dioxide,” she said.
Treatments
Badia noted that each patient should be treated based on their individual needs and concerns. The adult acne review by Dreno and colleagues contained a summary of the 2018 international consensus treatment recommendations from the Global Alliance to Improve Outcomes in Acne Group. The recommendations are as follows3:
Recommendation 1
Retinoids play an essential role in acne treatment, with a topical retinoid and benzoyl peroxide as first-line treatment for inflammatory acne and/or comedonal acne.
Recommendation 2
Systemic and topical antibiotics should be avoided as monotherapy.
Recommendation 3
Very severe (cystic and conglobata) acne should be treated with oral isotretinoin.
Recommendation 4
Patients should take oral isotretinoin until their acne clears. Total cumulative dosage to keep acne in remission needs more studies.
Recommendation 5
Use low-dose oral isotretinoin to minimize acne flares.
Recommendation 6
Maintenance therapy with a topical retinoid combined or not with benzoyl peroxide should be used for most patients. Avoid topical antibiotics for maintenance therapy.
Recommendation 7
Pregnant women and patients with acne and postinflammatory hyperpigmentation should be prescribed azelaic acid cream 20% or gel 15%.
Recommendation 8
Do not use devices (laser, intense pulsed light, photodynamic therapy) as first-line treatments for inflammatory acne.
Recommendation 9
In a small number of women 25 years and older, only the lower face is affected by acne. Topical retinoids with or without benzoyl peroxide should be used.
Recommendation 10
Starting treatment early minimizes the risk of scarring.
Newer Novel Treatments
Badia noted that acne therapies have come a long way.
“With concerns about antibacterial resistance on the rise, a new topical minocycline [Amzeeq] is the first of its kind to deliver antibiotic therapy with minimal systemic absorption,” she noted. “Another novel medication for acne is clascoterone cream 1% [Winlevi]. This medication is an antagonist of dihydrotestosterone and prohibits the production of sebum.” She explained that clascoterone is similar in structure to spironolactone but has minimal systemic antiandrogen effects and is safe for both men and women.
She added that topical retinoids continue to be “the gold standard in acne treatment” and that “many new formulations...have come out recently with age indications as young as 9 years old.”
Acne Prevention: Patient Guidance
Badia recommended advising patients of the following:
- Protect their skin by using a daily SPF with zinc oxide and by not actively tanning.
- Clean their faces daily with a gentle cleanser.
- Avoid products that contain alcohol, harsh exfoliants, and astringents that can irritate the skin and make acne worse.
- Avoid popping or picking acne lesions because this could lead to more acne and scarring.
References
- Dagnelie MA, Poinas A, Dréno B. What is new in adult acne for the last 2 years: focus on acne pathophysiology and treatments. Int J Dermatol. 2022;61(10):1205-1212. doi:10.1111/ijd.16220
- Tanghetti EA, Kawata AK, Daniels SR, Yeomans K, Burk CT, Callender VD. Understanding the burden of adult female acne. 2014;7(2):22-30. Accessed September 29, 2022. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3935648/
- Thiboutot DM, Dréno B, Abanmi A, et al. Practical management of acne for clinicians: an international consensus from the Global Alliance to Improve Outcomes in Acne. J Am Acad Dermatol. 2018;78(suppl 1):S1-S23.e1. doi:10.1016/j.jaad.2017.09.078

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.