- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Apremilast treatment in a patient with COVID-19
Author(s):
Case study finds no safety concerns, suggests possible benefit of apremilast for countering COVID-19 virus-induced inflammation.
The effect of existing pharmacotherapies on a patient’s risk of contracting COVID-19 and the clinical course of the viral infection has been of high interest and a topic for a number of published papers in the dermatology literature. In a recent Letter to the Editor appearing in the Journal of the European Academy of Dermatology and Venereology, dermatologists from the University of Cagliari, Cagliari, Italy, reported on a patient who developed a severe COVID-19 pulmonary infection while being treated with apremilast (Otezla, Amgen) for erythrodermic psoriasis.1
The patient also had recurrent brain oligodendroglioma that presented a contraindication to the use of most other therapies that would be used to control the erythrodermic psoriasis. One week after he had attended an appointment in a hospital clinic to be evaluated for brain radiotherapy, the patient developed symptoms of COVID-19, which included a high fever and severe cough. He was found to have bilateral interstitial pneumonia on radiographic imaging, and the diagnosis of COVID-19 was confirmed by a swab test for the coronavirus.
RELATED: COVID-19 impact in patients on biologics
The man was admitted to the hospital where he was started on antiviral and antibacterial medications. He was discharged home six days later, based on clinical resolution of his COVID-19 symptoms and two consecutive negative swabs for SARS-CoV2.
Laura Atzori, M.D., corresponding author of the article and associate professor of dermatology, University of Cagliari, told Dermatology Times, “Apremilast is a very interesting innovative drug that appears to be safe as a treatment for psoriasis and psoriatic arthritis in patients who may not be candidates for biologics because of their comorbidities. Although our experience involves a single case, it appears that secondary to its activity for decreasing the release of inflammatory cytokines, apremilast may also have a positive effect in patients with severe COVID-19 pneumonia.”
As an additional message, Dr. Atzori observed that the reported case underscores the importance of implementing care strategies for protecting vulnerable patients from contracting COVID-19.
“Patients with chronic inflammatory diseases, such as psoriasis, have challenged conventional management paradigms during the coronavirus SARS-2 pandemic,” she says. “Keeping patients home and ensuring that they remain on effective treatment to control their chronic skin disease is paramount so that they can avoid coming to the clinic where they may be at greater risk for exposure to COVID-19. Unfortunately because of his brain tumor, our patient was forced to continue receiving care in a hospital setting where we believe he contracted COVID-19.”
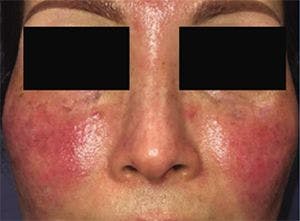
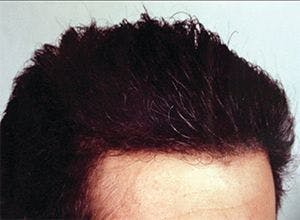
The patient was a 45-year-old obese man with a 10-year history of severe psoriatic arthritis that had been treated over the years with a number of traditional and biologic agents. He developed an erythrodermic flare of his psoriasis after starting treatment with temozolomide for a non-operable recurrence of his brain tumor. He was started on prednisone 50 mg/day and then apremilast 30 mg twice daily because of an insufficient response to the corticosteroid.
After starting apremilast, the patient’s skin condition improved, and the prednisone dose was successfully tapered to 12.5 mg daily. Treatment with apremilast was maintained during the patient’s hospitalization for COVID-19, and his psoriasis remained stable.
As discussed in their paper, Dr. Atzori and colleagues note that the patient’s rapid recovery from COVID-19 is particularly remarkable considering that he had multiple risk factors for a poor outcome. In that regard, his history supports the safety of apremilast in the setting of the coronavirus infection. It is also consistent with previous reports describing the safe use of apremilast in patients with other serious viral infections, including human immunodeficiency virus, hepatitis B virus, and hepatitis C virus.
The idea that apremilast may have had a therapeutic effect on the patient’s COVID-19 pneumonia and contributed to his fast improvement derives from knowledge of the drug’s activity for decreasing the production of certain cytokines that have been identified in the milieu of chemical mediators comprising the “cytokine storm” of COVID-19, including tumor necrosis factor-α and interleukin-6. In addition, apremilast was found in a preclinical model to prevent and reverse pulmonary inflammation induced by carfilzomib, a proteasome inhibitor used to treat relapsing or recurrent multiple myeloma.
“There has been interest in using tocilizumab, an interleukin-6 receptor antagonist, for the treatment of COVID-19. Considering the favorable safety profile of apremilast, we believe further studies are warranted to further understand its immunomodulating activities and potential role in the management of COVID-19,” Dr. Atzori says.
Disclosure:
Dr. Atzori and her colleagues report no relevant financial interests.
Reference:
1 Mugheddu C, Pizzatti L, Sanna S, Atzori L, Rongioletti F. COVID-19 pulmonary infection in erythrodermic psoriatic patient with oligodendroglioma: safety and compatibility of apremilast with critical intensive care management [published online ahead of print, 2020 May 9]. J Eur Acad Dermatol Venereol. 2020;10.1111/jdv.16625

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.