- Acne
- Actinic Keratosis
- Aesthetics
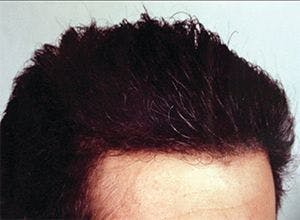
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
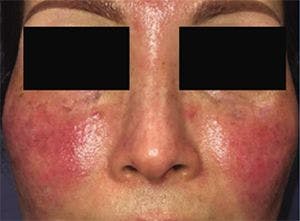
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
COVID-19 impact in patients on biologics
Author(s):
Treatment with biologics may worsen infection risk, not prognosis, according to findings from a case-control study comprised of more than 10 million residents of the Lombardia region of Italy.
Patients with psoriasis being treated with a biologic agent appear to be at increased risk for developing COVID-19, but not for progression to a severe form of the coronavirus infection, according to a report from Italian researchers. In a paper published online in the journal Dermatologic Therapy, Giovanni Damiani, M.D., and colleagues presented the findings from a case-control study they conducted to understand the effect of biologic treatment on COVID-19 risk and prognosis.1
In an unadjusted analysis, adult patients receiving a biologic or small molecule agent for treatment of moderate-to-severe plaque psoriasis had a statistically significant, 2.4-fold increased likelihood of having symptoms of COVID-19 compared with the control group, which was comprised of the more than 10 million residents of the Lombardia region of Italy.
RELATED: Apremilast treatment in a patient with COVID-19
The patients with psoriasis on a biologic or small molecule also had statistically significant increased risks for being hospitalized with COVID-19 (2.6-fold) and quarantined at home with the infection (8-fold). However, they were not more likely than the controls to have been admitted to an intensive care unit (ICU) because of COVID-19 or to have died from their disease.
Dr. Damiani is a clinical dermatologist, researcher at IRCCS Istituto Ortopedico Galeazzi, Milan, Italy, and director of the Young Dermatologists Italian Network.
“This is one of the first large studies conducted to understand the effect of biologic therapy on psoriasis patients during the COVID-19 outbreak," he says. "Its results are consistent with reports that biologics increase susceptibility to developing respiratory infections and correspond with evidence that biologic treatment may mitigate baseline airway inflammation that occurs in patients with psoriasis. In addition, our findings support the hypothesis that by inhibiting pro-inflammatory cytokines, a biologic might protect against progression of COVID-19 to a more severe stage.”
Dr. Damiani continues, “Based on our findings, we suggest that patients with psoriasis who are being treated with a biologic should be carefully monitored for symptoms of COVID-19 infection. However, because these individuals generally exhibit only the milder symptoms of the disease, it appears that the majority may be expected to be treated at home with follow-up via telemedicine or perhaps require a relatively short hospitalization.”
At the time the study was undertaken, the Lombardia region in Italy had the highest number of confirmed COVID-19 cases in Europe as well as the highest number of COVID-19-related hospitalizations and deaths. Subjects for inclusion in the study’s case cohort were identified from those receiving care at the psoriasis clinic in San Donato Hospital, Milan.
The study design reduces the potential for confounding variables, Dr. Damiani says of the strength, making it possible to present stronger conclusions. The case cohort resides in the same geographic region and have been exposed to the same potential environmental risk factors. All patients with psoriasis received the same teledermatology care from a single center by the same board-certified dermatologist using the same virtual visit criteria.
A total of 1,193 patients met the eligibility criteria for case inclusion that required age >18 years, diagnosis of moderate-to-severe plaque psoriasis for >1 year, participation in teledermatology, residence in Lombardia, and maintenance monotherapy with a biologic or small molecule approved for psoriasis. The most common classes of treatment being received were interleukin-17 inhibitors (45%), TNFα inhibitors (22%), and interleukin 12/23 inhibitors (20%).
Within the case cohort, 22 patients (1.8%) had a confirmed diagnosis of COVID-19, of which 17 were quarantined at home (1.4%) and 5 were hospitalized (0.4%). None of the case patients diagnosed with COVID-19 had been admitted to an ICU, developed the most severe stage of COVID-19 (stage III, hyperinflammation phase with extrapulmonary manifestations driven by a cytokine storm), or had died from the infection.
Among the controls, 54,801 were COVID-19 positive, 16,042 were quarantined at home, 11,796 were hospitalized for their infection, 1,236 were in the ICU, and 10,222 had died.
Discussing the study’s limitations, Dr. Damiani observed that in the case cohort, only 89 patients (7.5%) were on a small molecule drug.
“None of the patients on a small molecule biologic therapy developed COVID-19, but because they represented the smallest proportion of the treatment cohort, future studies should be done to evaluate more in-depth the potential impact of small molecule biologic therapy on COVID-19,” he says.
Dr. Damiani also notes that information for individuals in the control group were obtained using publicly available data from the Lombardia region that could not be independently validated. In addition, the between-group comparisons were unadjusted and done without any stratification of subjects by age group or matching by sex.
Reference:
1 Damiani G, et al. Biologics increase the risk of SARS-CoV-2 infection and hospitalization, but not ICU admission and death: Real-life data from a large cohort during red-zone declaration. Dermatol Ther. 2020;e13475. [Epub May 1, 2020.]

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.