- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
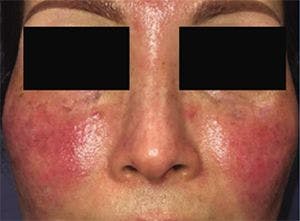
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
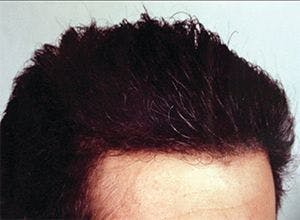
Hair transplantation outcomes improve
Author(s):
Excellent results can be achieved using either follicular unit extraction/excision (FUE) or follicular unit transplantation/transfer (FUT) for hair transplantation. Technique selection should consider the unique needs, considerations, and preferences of the patient, experts say.
The history of hair transplantation surgery is characterized by an ongoing evolution in terms of techniques and technologies. Introduction of follicular unit extraction/excision (FUE) in the early 2000s was a revolutionary event that created a lot of excitement and was expected by some to totally replace follicular unit transplantation/transfer (FUT).
Current best practice now recognizes that both FUE and FUT have a place in the hair restoration surgeon’s toolbox, according to dermatologists who specialize in hair loss and hair restoration.
Dr. Leavitt
“Both FUE and FUT have pros and cons. Each may be preferred in a given patient at a given time depending on multiple factors, and because of changing circumstances, they may both be used during an individual’s lifetime to obtain optimal results,” says Matt Leavitt, D.O., founder and CEO, Advanced Dermatology and Cosmetic Surgery, and Executive Medical Advisor for Bosley, Maitland, Fla.
RELATED: Facts and trends in hair restoration
Natalie Kash, M.D., is a board-certified dermatologist completing a hair restoration surgery fellowship under Dr. Leavitt. She adds, “A combination approach that augments hair transplant surgery with other modalities can also be key for optimizing short-term and long-term outcomes.”
Dr. Leavitt and Dr. Kash spoke to Dermatology Times about the current state-of-the-art techniques in hair restoration surgery.
Individualizing the plan
The list of variables that are considered when planning hair transplantation surgery include the patient’s age, amount of donor hair available, and expected future hair loss based on family history. In addition, the decision takes into account the patient’s hair color and length, scarring risk, scalp tightness, and willingness for social downtime. Cost may also be an issue.
Comparing FUT and FUE, Dr. Leavitt says that FUT is less expensive than FUE because FUT is both quicker to perform and often yields a higher number of grafts in a single session.
“When harvesting the grafts for FUT, it is easier for less experienced hair surgeons to visualize the direction of individual follicular units, and; therefore, FUT may be associated with a lower rate of follicular transection compared with FUE,” he explains.
Unlike FUE, FUT allows patients to keep the hair long at the donor site on the day of surgery.
On the other hand, depending on the color of their hair and other factors, patients may need to keep their hair longer at the donor site to cover the FUT linear scar after surgery.
Compared with FUE, FUT is also a more invasive procedure overall and has the potential for more complications.
Dr. Kash

“FUT is associated with more bleeding than FUE, a greater risk for hypertrophic scarring, and carries a higher potential for patients to perceive tightness or discomfort in the postoperative period,” Dr. Kash says.
RELATED: First-line treatment for hair loss
FUE avoids the downsides of FUT, but has its own list of disadvantages. Compared with FUT, it can be more difficult to obtain as many high-quality grafts in one FUE session, particularly when the procedure is not performed by expert hands.
“Unless they are using an expensive piece of equipment for harvesting the grafts, beginning surgeons might struggle with preserving the natural anatomy of the hair follicle when performing FUE,” Dr. Leavitt says.
With serial FUE sessions, it becomes increasingly difficult to obtain a high graft count as prior FUE scars alter the direction of the remaining hairs, and it is important to avoid overharvesting the donor area.
“FUE is sometimes described as scarless, but that is a misrepresentation. Although it does not produce a linear scar, it creates numerous small scars, and the resulting scalp contraction can alter the direction of surrounding hairs,” Dr. Kash explains.
With all of these issues in mind, FUE tends to be more attractive to patients who like to wear their hair shorter and those who want to avoid a linear scar. Because of the nature of the procedure, FUE is also very well-suited for people needing a limited number of grafts to address a localized area of hair loss such as for the treatment of the eyebrows or a scar on the scalp.
In contrast, because it is able to harvest more grafts more easily, FUT will be a better option formen and women with more advanced androgenetic alopecia, ie., men with Norwood stage 4-6 balding or women with Ludwig type 2 or higher.
Future-based planning
For a variety of reasons, patients often have more than one hair transplantation procedure over their lifetime.
“Hair loss is dynamic, and an individual’s trajectory continues to evolve over time based on numerous environmental factors, genetics, their overall health, and age. Age-related changes also occur, including decrease in hair density, pigmentation, and mass,” Dr. Leavitt explains.
“Furthermore, hair restoration can be an addicting pleasure for some people — the more hair they have, the more they want.”
Whereas patients may have FUE or FUT initially, the other procedure may be more appropriate later on taking into account changing patient preferences and clinical characteristics that can affect the potential to obtain the maximal number of quality grafts. For example, a patient who had a FUT procedure may not be a candidate for a second FUT later if scalp tightness precludes the ability to obtain another strip. Or, the patient may simply not want to have another linear scar. Someone whose first transplant was an FUE procedure might be a better candidate for FUT in the future to avoid overharvesting of follicular units from a donor area.
Anticipating ongoing loss is a critical consideration when performing any hair transplantation surgery. With that in mind, Dr. Leavitt says that optimizing long-term outcomes depends on transplanting hairs not only in areas where there is significant balding, but also at sites where there is less significant thinning. This approach will allow a natural transition of hair density as hair loss continues over time.
“Placing the grafts only in the areas where hair loss is worse puts a patient at later risk for developing an appearance that does not exist in nature,” Dr. Leavitt says.
Adjuncts for optimizing results
Even patients who choose hair transplantation to address hair loss should be on medical therapy to maintain their existing hair. The benefit of this combination approach was demonstrated in a double-blind study that randomized men to treatment with finasteride or placebo for one month before and 48 weeks after undergoing hair transplantation1,” Dr. Leavitt says.
“We do not yet have a way of creating more donor hair, and the areas of hair on the head that are not susceptible to hormone-related loss are limited to sites on the back and sides of the head in men and may be even smaller in women. Therefore, it is important to preserve as much donor hair as possible,” he explains.
Dr. Kash adds, “Adding medical therapy for a patient who has had surgical treatment for hair loss is part of a good long-term plan. Many patients who have surgery are just in their 20s or 30s and may continue to seek treatment into their 70s. Maintaining donor hairs is important to give these patients an optimal result over time.”
Combination approaches
Aside from incorporating medical therapy, hair transplantation surgery may be combined with other modalities to achieve the best outcomes, Dr. Kash says.
Platelet rich plasma (PRP) injection is one option. Delivered at the recipient site prior to placing the grafts, PRP has potential benefits for promoting graft survival and accelerating healing.
“In the future, exosome therapy, which is an emerging injectable treatment being investigated for its potential to promote hair restoration and prevent hair loss, might also be combined with hair transplantation,” Dr. Kash says.
Scalp micropigmentation is another technique that could be used in patients having hair transplantation. This procedure involves the application of permanent ink to the scalp using microfine needles.
Done in the area where hair is transplanted or elsewhere on the scalp, scalp micropigmentation can create an illusion of thicker fuller hair by reducing scalp visibility. It might also be used to add definition to the hairline or to camouflage the linear scar created with a FUT.
Opportunities for treating scarring alopecia
Advances in hair transplantation also include the possibility of success in patients with scarring alopecia who in the past were thought to be poor candidates for the surgery. However, the scarring condition must be medically stabilized and inactive for at least two years and up to five years according to some experts. In addition, it is important that the hair restoration surgeon is comfortable and experienced with the nuances of how and when to perform hair transplantation in patients with a history of scarring alopecia.
Dr. Kash explained that multiple additional steps are often done prior to performing hair restoration surgery in patients with scarring alopecia to rule out disease activity. These include a careful clinical examination of the scalp with trichoscopy along with scalp biopsy in many cases for histological confirmation of quiescence. Test grafts may also be appropriate in some cases.
Patients with scarring alopecia who are considered candidates for surgical restoration also need to be counseled about the importance of continuing medical treatment for their condition and maintaining regular follow-up with their managing dermatologist. They should also be told that there is a higher rate of graft failure in patients with scarring alopecia versus androgenetic alopecia, even if the scarring condition has been inactive for years.
“Patients must understand that medical management must be ongoing because surgery will not address the cause of the alopecia, and there is also a need to set appropriate expectations for their outcome,” Dr. Kash says.
Disclosures:
Neither Dr. Leavitt nor Dr. Kash report any relevant financial interests.
Reference:
Leavitt M, Perez-meza D, Rao NA, Barusco M, Kaufman KD, Ziering C. Effects of finasteride (1 mg) on hair transplant. Dermatol Surg. 2005;31(10):1268-76.

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.