- Acne
- Actinic Keratosis
- Aesthetics
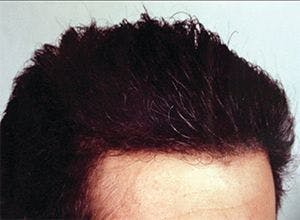
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
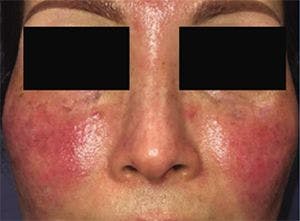
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Dermatologists on New York City's COVID-19 frontlines
Author(s):
Eighteen residents and fellows in the throes of their dermatology training volunteered at the frontlines of overwhelmed Bronx-based hospitals during the height of the COVID-19 pandemic, gaining a crash course in crisis medicine and infectious diseases.
Eighteen residents and fellows in the midst of their dermatology training at New York City’s Albert Einstein College of Medicine didn’t anticipate a crash course in crisis medicine and infectious diseases. But when they got the call to help at the frontlines of overwhelmed Bronx-based hospitals during the height of the COVID-19 pandemic, they stepped up and volunteered.
At the height of the crisis, hospitals in the Bronx in the Montefiore Health System and the Health and Hospitals Corporation network had more than 2,000 patients with COVID-19. The medical floors became overwhelmed and put out a call for volunteers in all medical specialties, according to Steven R. Cohen, M.D., M.P.H., professor and chief of dermatology at Albert Einstein College of Medicine and Montefiore Medical Center.
“Pretty much, it was all hands on deck. We have 20 residents and two fellows. Virtually everybody was involved in some way. They were totally heroic,” Dr. Cohen says.
Emily Hejazi, M.D., a fourth-year dermatology resident at Albert Einstein College of Medicine/Montefiore, was deployed to Wakefield Hospital, a community hospital, to work on the COVID-19 ward as a general medicine doctor.
“We were responsible for the complete care of the patients with COVID-19, from their admission to the floor to their discharge or death. That included monitoring their labs, monitoring their respiratory status, providing them with medications, speaking with the families. We did everything for the patients,” Dr. Hejazi says.
It had been about five years since Dr. Hejazi had end-of-life conversations with families.
“It was really challenging at first to remember those skills. Having end-of-life conversations is not something I’m used to doing anymore as a dermatologist. But it did come back to me after a couple of days. As physicians, this is what we do, and those skills, even if we haven’t used them in several years, they’re still there,” she says.
Volunteering, no easy decision
Einstein’s dermatology residents and fellows were aware that their decision to volunteer on hospital medical wards would throw them into providing medical care for which they weren’t adequately trained and would put them at risk for contracting the virus.
Andrea Waldman, M.D., a fourth-year dermatology resident with Albert Einstein College of Medicine, volunteered but was concerned about being able to care for adults. Her experience was in pediatrics before training in dermatology.
“I realized that I could do a lot more to help as a doctor than I realized I could,” Dr. Waldman says. “I basically functioned as a medicine intern under the supervision of the medicine resident and the attending.”
None of the doctors on Dr. Waldman’s team intended to go into medicine, but each offered a different perspective in the crisis, she says.
“Our attending doctor was deployed from Florida as a military reserve attending with the Air Force. The other people on my team were a medicine resident, two medicine interns, a radiology resident and an OB/gyn physician assistant. The medicine resident is going into surgery, the two interns in medicine are going into radiology and neurology,” Dr. Waldman says.
Dr. Hejazi hesitated about volunteering because she has a family to think about, including a breastfeeding 13-month-old daughter and 3.5-year-old son. However, she says her first instinct after hearing the call to residents was to go.
“We have a responsibility to help people anyway that we can and I really wanted to volunteer right away. But having a family, there was a concern about exposing my family to the virus,” Dr. Hejazi says.
Dr. Hejazi says she took a few weeks to wait and see. But as things got worse in New York City, it became clear that she needed to help. Dr. Hejazi and her husband decided that they would remain together in their New York City apartment to weather the storm. She’d come home after the day’s work to a meticulous infection control routine. Dr. Hejazi says she’d walk through the doors to excited children and a husband who managed everything while she was gone but there would be no hugging until she carefully took off her hospital garb, showered and started the laundry.
“I think it was pretty effective for us. No one got sick, thank God, so far,” she says.
Five of the 18 volunteers, however, did get COVID-19 and suffered symptoms.
Chief dermatology resident Claudia Hossain, M.D., worked most of the way through her COVID-19 infection, Dr. Cohen recalls.
“Claudia didn’t know she had it but wasn’t feeling great. Finally, she got tested. The results came back and she was positive, so we made her rest. She rested for about three days and went back to work. She was afebrile but had symptoms,” Dr. Cohen says. “One of the first residents who got infected spent 16 days in bed. We didn’t have anybody, thank God, with mysterious pulmonary debilitation, but we really had people who were sick. It’s hard to explain the sacrifices the residents made.”
Anyone exposed to an infected person would go into quarantine in the beginning stages of the pandemic. As it progressed to where basically everything, including the hospital cafeterias, were converted into places for COVID-19 beds, healthcare providers could work even if they had symptoms as long as they wore protective gear, according to Dr. Cohen.
“People in other parts of the country just don’t realize,” Dr. Cohen says.
Being sick wasn’t what Dr. Hossain talked about during the Dermatology Times’ interview. She talked about what a rewarding experience it was to be part of a multispecialty team on the wards, helping to fight the deadly virus.
“I got to help my team and teach. I got to take care of COVID patients and help deal with the volume, and contribute to taking care of our community, which was pretty great,” Dr. Hossain says.
Some of the doctors suffered financial hardships, and many found personal protective equipment (PPE) lacking. So, these residents and fellows started a GoFundMe page to raise money to help financially troubled colleagues and buy needed PPE. They raised nearly $19,000.
The call to COVID duty also derailed training. Still, many of Einstein’s fourth-year dermatology residents are planning to take their boards in July.
It won’t be an easy transition, according to Dr. Hejazi. Fourth-year residents usually use the end of their training to study and gear up for boards. But working 80- to 90-hour weeks on COVID-19 floors for weeks didn’t leave a lot of time or energy for studying or thinking about dermatology, she says.
Some of the residents did see patients with skin manifestations, including retiform purpura plaque and, oddly, chilblains, according to Dr. Cohen.
“Chilblains are kind of the stock-in-trade of British dermatologists because they have a lot of that in their cold, wet, moist environment. It’s quite a shock that many of the patients who have coronavirus were developing chilblains,” Dr. Cohen says.
Other than the occasional cutaneous finding, there weren’t similarities between what happened during the pandemic to what occurs in residency training, according to Dr. Cohen.
“These residents were basically immersed in hardcore medicine. I don’t know if it was the most enriching experience from a dermatologic perspective," he says. "You need to look at it from a humanitarian perspective.”
For dermato-pharmacology fellow José Jaller, M.D., the crisis enriched his future in research. Today, Dr. Jaller spends about 70% of his time doing groundbreaking research for Montefiore Hospital’s department of infectious diseases in remdesivir (GS-5734, Gilead Sciences) and convalescent plasma trials for COVID-19.
Montefiore is one of 70 sites worldwide involved in the remdesivir trial. With New York City being an epicenter, the Bronx hospital had about 10% of the patients in the study that led to the FDA’s granting emergency use for treating COVID-19 as of May 1.
Dr. Jaller says the experience has been quite different than the research he does in dermatology on eczema, psoriasis, alopecia and other cutaneous conditions.
Most dermatology patients will not die if they don't get treatment, he says. That’s not the case in the initial remdesivir study on hospitalized patients with COVID-19, which showed patients who received remdesivir versus placebo had a significant reduction in hospital stays and a trend toward increased survival.
“That’s something that really impacts you. You are really influencing the patient’s life in the short-term,” Dr. Jaller says.
Dr. Jaller says he plans to continue to work in the COVID-19 setting even if the pandemic subsides. He’s starting a dermatology residency in 2021 and will complete one year of internal medicine starting in July.
“So, I’m actually going to go to the floors and will probably be dealing with this virus for my entire intern year on the floors,” he says.
Dr. Jaller is now involved in the second phase of remdesivir trials for COVID-19 treatment. All patients will receive remdesivir, with no placebo group. Researchers will add a Janus kinase (JAK) inhibitor to the treatment regimen. Researchers are also studying JAK inhibitors to treat various dermatologic conditions.
Lessons learned
Despite the challenges, these residents say there was a lot of good the emerged.
Dr. Waldman says she walked away from the experience realizing that she was there for the patients.
“They couldn’t have visitors. A lot of my patients were elderly, so you were really their lifeline. I would spend time with them, and I really bonded with my patients while taking care of them,” Dr. Waldman says.
The experience helped to make many of the frontline providers better people and better physicians, according to Dr. Hejazi.
“Even though it has been a difficult experience and I’ve seen things, experienced things and made decisions that I never really imagined I would, it shaped me as a physician. I think it made me a more compassionate and understanding physician. The things I’ve learned in these past few months will forever change the way I practice in a good way,” Dr. Hejazi says.
During the worst days of the pandemic, Dr. Cohen never heard a resident or fellow say, “I’m not going to do this.” Or “I didn’t sign up for this.” Some worked the nightshift, without a complaint.
“I have to say our residents are astonishing, with a total willingness to do whatever needed to be done,” Dr. Cohen says. “They truly define the expression, ‘heroism.’”

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.