- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Skin manifestations an early sign of rare hematologic cancer
Author(s):
Blastic plasmacytoid dendritic cell neoplasm isn’t a skin cancer. Yet, dermatologists might be the first providers to encounter these patients.
Dr. Geskin, M.D.

Blastic plasmacytoid dendritic cell neoplasm isn’t a skin cancer. Yet, dermatologists might be the first providers to encounter these patients.
Blastic plasmacytoid dendritic cell neoplasm is a rare, aggressive hematologic malignancy that may manifest on the skin and may have leukemic dissemination,” Larisa J. Geskin, M.D., president of the International Society for Cutaneous Lymphomas, told Dermatology Times. “It is derived from myeloid-derived resting plasmacytoid dendritic cells (type 2 dendritic cells), thus it has ‘myeloid’ origin. Because of its early manifestations on the skin, dermatologists are well positioned to diagnose it early.”
Awareness about this cancer is lacking. Blastic plasmacytoid dendritic cell neoplasm, which most commonly impacts people in their 60s and 70s, is often misdiagnosed and under-reported. There’s little data about it and limited options for treatment, according to the Leukemia and Lymphoma Society.
The cancer’s immunophenotypic signature
Dr. Geskin, associate professor of dermatology and director of the Comprehensive Cutaneous Oncology Center at Columbia University’s Department of Dermatology, and colleagues reported in observation published April 2018 in JAMA Dermatology on a man in his 70s diagnosed with blastic plasmacytoid dendritic cell neoplasm.
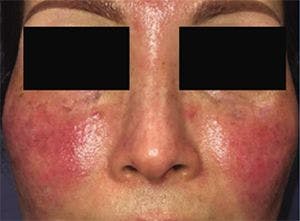
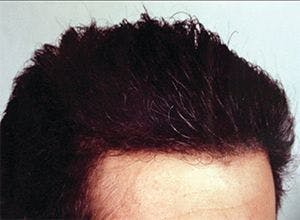
The patient first noticed two purple asymptomatic bumps on his chest. By two weeks, the bumps grew and spread to the patient’s back, face and scalp. He had a skin biopsy but developed severe abdominal pain before being diagnosed and presented to the emergency department for the pain.
The doctor there noted many nontender purpuric nodules and plaques covering the man’s forehead, trunk and back. A CT scan showed marked splenomegaly and diffuse intraabdominal and intrathoracic lymphadenopathy. Laboratory values revealed an elevated white blood cell count, high lactate dehydrogenase level, low platelet count and low hemoglobin level.
Other tests supported a blastic plasmacytoid dendritic cell neoplasm diagnosis, including a bone-marrow biopsy. Among other things, the biopsy showed CD4, CD56 and CD123 positivity. The initial skin biopsy results showed the immunophenotype was the same as the bone-marrow biopsy except for being CD56−, the authors wrote.
Blastic plasmacytoid dendritic cell neoplasm’s pathology characteristically expresses CD4+ with CD123 and either BDCA2 or TCL1, according to Dr. Geskin.
“These tumors frequently express CD56 and differential staining should be performed by path laboratory. Pathological differential diagnosis including cutaneous T-cell lymphoma (CTCL), subcutaneous panniculitis like T-cell lymphoma, nasal-type extranodal NK/T-cell lymphoma and CD56+ acute myeloid leukemia,” according to Dr. Geskin.
Interestingly, this case shows there are rare variants in the cancer’s immunophenotypic signature, according to the authors. Researchers have also noted immunohistochemical variations in a small number of blastic plasmacytoid dendritic cell neoplasm patients.
“… the observed phenotypic heterogeneity in this case suggests that obtaining biopsy specimens from different sites might be necessary in a patient with putative [blastic plasmacytoid dendritic cell neoplasm] to maximize the chance of correct diagnosis,” they wrote.
The relevance of skin findings
Skin findings do not always correlate with disease stage in blastic plasmacytoid dendritic cell neoplasm patients. And cutaneous clues may be absent in leukemic blastic plasmacytoid dendritic cell neoplasm, according to Dr. Geskin.
But skin manifestations are common with this cancer. According to the Leukemia and Lymphoma Society, skin is involved in 80% of blastic plasmacytoid dendritic cell neoplasm cases.
Blastic plasmacytoid dendritic cell neoplasm may present on the skin with nonspecific brown or purple/violaceous bruise-like lesions, plaques, or tumors, Dr. Geskin said.
“There may be a single lesion or, most commonly, multiple,” she said. “Because there is no pathognomonic finding of [blastic plasmacytoid dendritic cell neoplasm] clinically, physicians have to have high level of suspicion and low threshold for offering a biopsy to the patients. Another important factor is evaluation of the specimen by a pathology laboratory, which is familiar with an entity, so appropriate studies can be quickly done on the specimen, to expedite diagnosis and patient’s care.”
Tagraxofusp-erzs (Elzonris, Stemline) is approved for blastic plasmacytoid dendritic cell neoplasm treatment in adult and pediatric patients two years and older. Patients tend to respond for only a short time to treatment, so the recommendation is to evaluate these patients for allogeneic hematopoietic stem cell transplant and begin searching for a donor as soon as possible, according to the Leukemia and Lymphoma Society
Disclosures:
Dr. Geskin was an investigator on the Stemline Therapeutics study for blastic plasmacytoid dendritic cell neoplasm.
References:
Lopez AT, Shaw KS, Yamany T, Husain S, Geskin L. Immunophenotypic CD56 Variation Within a Single Patient With Blastic Plasmacytoid Dendritic Cell Neoplasm. JAMA Dermatol. 2018;154(4):492-494.

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.